Easy Way to Learn Nursing Lab Values
Knowing the different normal lab values is an important step in making an informed clinical decision as a nurse. Diagnostic and laboratory tests are tools that provide invaluable insights and information about the patient. Lab tests are used to help confirm a diagnosis, monitor an illness, and the patient's response to treatment.
In the NCLEX, some questions supply laboratory results with no indication of the normal lab levels so you'll have to familiarize yourself with them. NCLEX will not give you values that are within the normal range. Questions will usually include critical lab values and it's a matter of identifying if it's within normal range or not.
Please note that laboratory values may vary from agency to agency.
Download Free Normal Lab Values Cheat Sheet
You can download a summary or cheat sheet of this normal laboratory values guide below.

Simply click on the images above to get the full resolution format that you can use for printing or sharing. Feel free to share these cheat sheets for normal lab values!
Phases of Diagnostic Testing
Diagnostic testing involves three phases: pretest, intratest, and post-test. Nurses have responsibilities for each phase of diagnostic testing.
Before the procedure
In the pretest, the main focus is on preparing the client for the diagnostic procedure. Responsibilities during pretest include:
- Assessment of the patient to assist in determining precautions.
- Preparation of the equipment and supplies needed.
- Preparation of a consent form, if required.
- Providing information and answering client questions about the procedure.
During the procedure
During intratest, the main focus is specimen collection and performing or assisting with certain diagnostic procedures. Additional responsibilities during intratest are:
- Use of standard precautions or sterile technique if necessary.
- Providing emotional support to the patient and monitoring the patient's response during the procedure.
- Ensuring the correct labeling, storage, and transportation of the specimen.
After the procedure
During the last part of diagnostic testing, the nursing care revolves around observations and follow-up activities for the patient. For example, if a contrast media was injected during a CT scan, the nurse should encourage the patient to increase fluid intake to promote excretion of the dye. Additional responsibilities during post-test include:
- Compare the previous and current test results
- Reporting of the results to the appropriate members of the healthcare team.
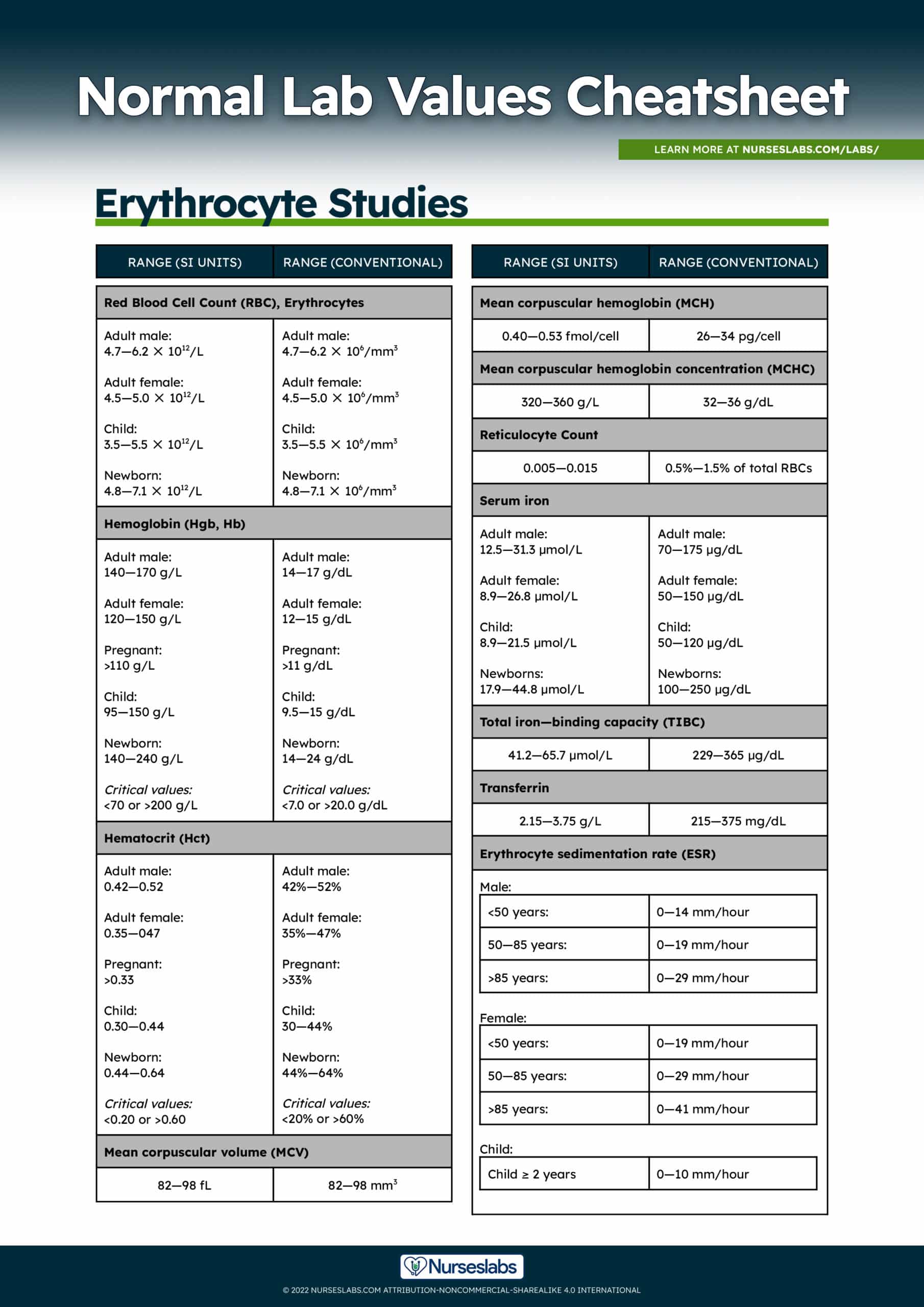
Erythrocyte Studies Normal Lab Values
Here are the normal lab values related to erythrocyte studies which include hemoglobin, hematocrit, red blood cell count, serum iron, and erythrocyte sedimentation rate. Venous blood is used as a specimen for complete blood count (CBC) which is a basic screening test that is frequently ordered to give an idea about the health of a patient.
Red Blood Cells (RBC) Normal Lab Values
Red blood cells or erythrocytes transport oxygen from the lungs to the bodily tissues. RBCs are produced in the red bone marrow, can survive in the peripheral blood for 120 days, and are removed from the blood through the bone marrow, liver, and spleen.
Indications of RBC count:
- Helps in diagnosing anemia and blood dyscrasia.
Normal values for red blood cell count:
| Range (SI Units) | Range (Conventional) | |
|---|---|---|
| Adult male | 4.7—6.2 ✕ 1012/L | 4.7—6.2 ✕ 106/mm3 |
| Adult female | 4.5—5.0 ✕ 1012/L | 4.5—5.0 ✕ 106/mm3 |
| Child | 3.5—5.5 ✕ 1012/L | 3.5—5.5 ✕ 106/mm3 |
| Newborn | 4.8—7.1 ✕ 1012/L | 4.8—7.1 ✕ 106/mm3 |
Hemoglobin (Hgb)
Hemoglobin is the protein component of red blood cells that serves as a vehicle for oxygen and carbon dioxide transport. It is composed of a pigment (heme) which carries iron, and a protein (globin). The hemoglobin test is a measure of the total amount of hemoglobin in the blood.
Indications of hemoglobin count:
- Hemoglobin count is indicated to help measure the severity of anemia (low hemoglobin) or polycythemia (high hemoglobin).
- Monitor the effectiveness of a therapeutic regimen.
Normal and critical values chart for hemoglobin count:
| Range (SI Units) | Range (Conventional) | |
|---|---|---|
| Adult male | 140—170 g/L | 14—17 g/dL |
| Adult female | 120—150 g/L | 12—15 g/dL |
| Pregnant | >110 g/L | >11 g/dL |
| Child | 95—150 g/L | 9.5—15 g/dL |
| Newborn | 140—240 g/L | 14—24 g/dL |
| Critical values | <70 or >200 g/L | <7.0 or >20.0 g/dL |
Hematocrit (Hct)
Hematocrit or packed cell volume (Hct, PCV, or crit) represents the percentage of the total blood volume that is made up of the red blood cell (RBC).
Normal and critical values for hematocrit count:
| Range (SI Units) | Range (Conventional) | |
|---|---|---|
| Adult male | 0.42—0.52 | 42%—52% |
| Adult female | 0.35—047 | 35%—47% |
| Pregnant | >0.33 (>33%) | >33% |
| Child | 0.30—0.44 | 30—44% |
| Newborn | 0.44—0.64 | 44%—64% |
| Critical values | <0.20 or >0.60 | <20% or >60% |
Increased hematocrit levels may indicate:
- Burns
- Chronic obstructive pulmonary disease
- Congenital heart disease
- Dehydration
- Eclampsia
- Erythrocytosis
- Polycythemia Vera
- Severe dehydration
Decreased hematocrit levels may indicate:
- Anemia
- Bone marrow failure
- Hemoglobinopathy
- Hemolytic reaction
- Hemorrhage
- Hyperthyroidism
- Leukemia
- Liver cirrhosis
- Malnutrition
- Multiple myelomas
- Normal pregnancy
- Nutritional deficiency
- Rheumatoid arthritis
Red Blood Cell Indices
Red blood cell indicates (RBC Indices) determine the characteristics of an RBC. It is useful in diagnosing pernicious and iron deficiency anemias and other liver diseases.
- Mean corpuscular volume (MCV): The average size of the individual RBC.
- Mean corpuscular hemoglobin (MCH): The amount of Hgb present in one cell.
- Mean corpuscular hemoglobin concentration (MCHC): The proportion of each cell occupied by the Hgb.
Normal Lab Values for RBC Indices are:
| Range (SI Units) | Range (Conventional) | |
|---|---|---|
| Mean corpuscular volume (MCV) | 82—98 fL | 82—98 mm3 |
| Mean corpuscular hemoglobin (MCH) | 0.40—0.53 fmol/cell | 26—34 pg/cel |
| Mean corpuscular hemoglobin concentration (MCHC) | 320—360 g/L | 32—36 g/dL |
| Reticulocyte Count | 0.005—0.015 | 0.5%—1.5% of total RBCs |
Serum Iron (Fe)
Iron is essential for the production of blood helps transport oxygen from the lungs to the tissues and carbon dioxide from the tissues to the lungs.
Normal lab values for serum iron:
| Range (SI Units) | Range (Conventional) | |
|---|---|---|
| Adult male | 12.5—31.3 µmol/L | 70—175 µg/dL |
| Adult female | 8.9—26.8 µmol/L | 50—150 µg/dL |
| Child | 8.9—21.5 µmol/L | 50—120 µg/dL |
| Newborn | 17.9—44.8 µmol/L | 100—250 µg/dL |
| Total iron—binding capacity (TIBC) | 41.2—65.7 µmol/L | 229—365 µg/dL |
| Transferrin | 2.15—3.75 g/L | 215—375 mg/dL |
Indication of serum iron:
- Helps in diagnosing anemia and hemolytic disorder.
Increased serum iron levels may indicate:
- Hemochromatosis
- Hemosiderosis
- Hemolytic anemia
- Hepatic necrosis
- Hepatitis
- Iron poisoning
- Lead toxicity
- Massive transfusion
Decreased serum iron levels:
- Chronic blood loss
- Chronic gastrointestinal blood loss
- Chronic hematuria
- Chronic pathologic menstruation
- Inadequate absorption of iron
- Iron deficiency anemia
- Lack of iron in the diet
- Neoplasia
- Pregnancy (late stages)
Nursing considerations for serum iron:
- Recent intake of a meal containing high iron content may affect the results.
- Drugs that may cause decreased iron levels include adrenocorticotropic hormone, cholestyramine, colchicine, deferoxamine, and testosterone.
- Drugs that may cause increased iron levels include dextrans, ethanol, estrogens, iron preparations, methyldopa, and oral contraceptives.
Erythrocyte Sedimentation Rate (ESR)
Erythrocyte sedimentation rate (ESR) is a measurement of the rate at which erythrocytes settle in a blood sample within one hour.
Normal lab values for erythrocyte sedimentation rate:
| Age | ESR | |
|---|---|---|
| Male | <50 years: | 0—14 mm/hour |
| 50—85 years: | 0—19 mm/hour | |
| >85 years: | 0—29 mm/hour | |
| Female | <50 years: | 0—19 mm/hour |
| 50—85 years: | 0—29 mm/hour | |
| >85 years: | 0—41 mm/hour | |
| Child | ≥ 2 years | 0—10 mm/hour |
Indication for Erythrocyte Sedimentation Rate:
- Assist in the diagnosis of conditions related to acute and chronic infection, inflammation, and tissue necrosis or infarction.
Increased ESR levels may indicate:
- Bacterial infection
- Chronic renal failure
- Hyperfibrinogenemia
- Inflammatory disease
- Macroglobulinemia
- Malignant diseases
- Severe anemias such as vitamin B12 deficiency or iron deficiency
Decreased ESR levels may indicate:
- Hypofibrinogenemia
- Polycythemia vera
- Sickle cell anemia
- Spherocytosis
Nursing consideration
- Fasting is not required
- Fatty meal prior extraction may cause plasma alterations
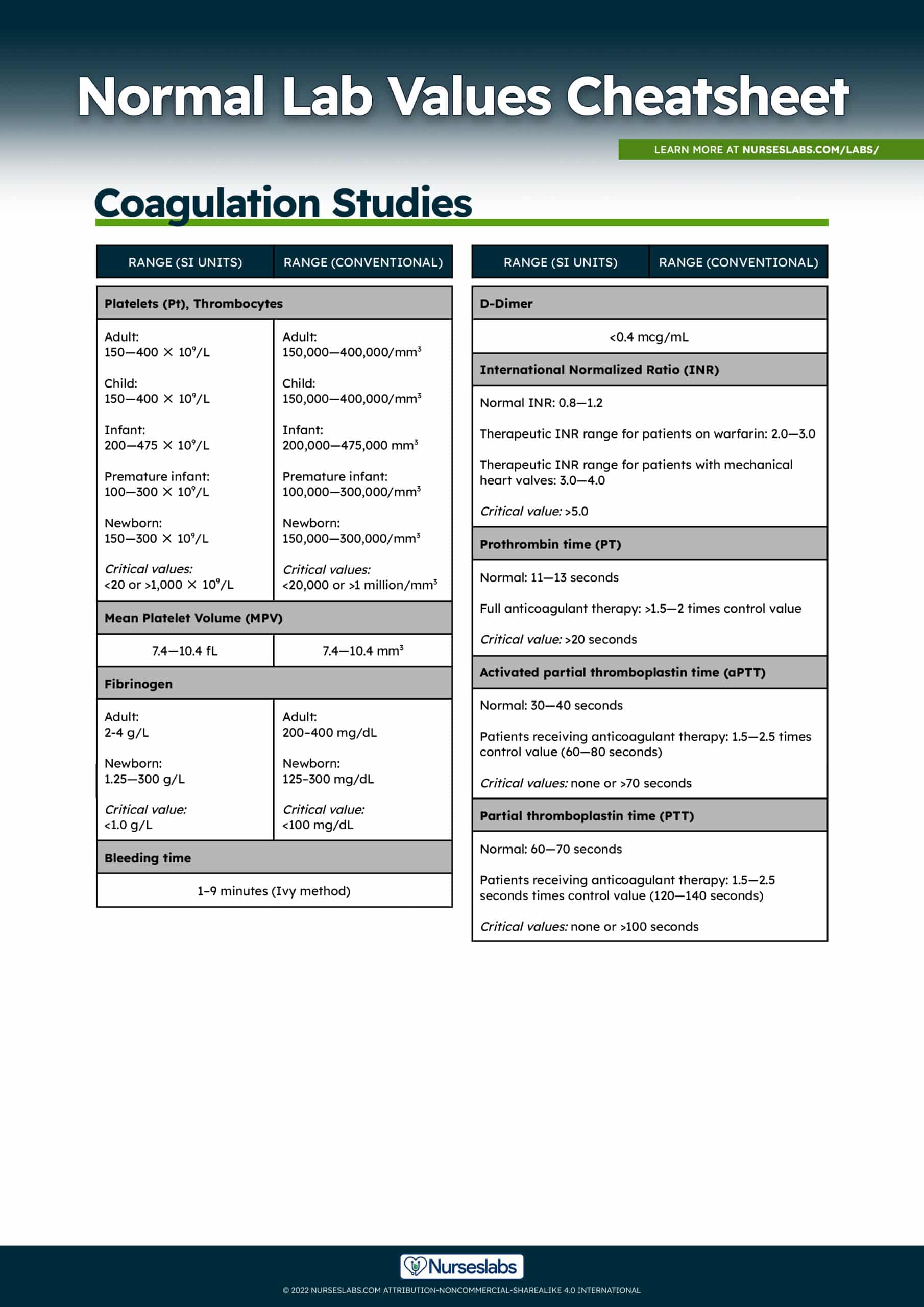
Coagulation Studies Normal Lab Values
Physicians order coagulation studies such as platelet count, activated partial thromboplastin time, prothrombin time, international normalized ratio, bleeding time, and D-dimer to evaluate the clotting function of an individual. In this section, we'll discuss the indications and nursing implications of each lab test.
Platelets (Pt), Mean Platelet Volume (MPV), Fibrinogen
Platelets are produced in the bone marrow and play a role in hemostasis. Platelets function in hemostatic plug formation, clot retraction, and coagulation factor activation.
Normal and critical values for platelet count and mean platelet volume:
| Range (SI Unit) | Range (Conventional) | |
|---|---|---|
| Adult | 150—400 ✕ 109/L | 150,000—400,000/mm3 |
| Child | 150—400 ✕ 109/L | 150,000—400,000/mm3 |
| Infant | 200—475 ✕ 109/L | 200,000—475,000 mm3 |
| Premature infant | 100—300 ✕ 109/L | 100,000—300,000/mm |
| Newborn | 150—300 ✕ 109/L | 150,000—300,000/mm3 |
| Critical values | <20 or >1,000 ✕ 109/L | <20,000 or >1 million/mm3 |
| Mean Platelet Volume (MPV) | 7.4—10.4 fL | 7.4—10.4 mm3 |
Normal and critical values for fibrinogen:
| Range | |
|---|---|
| Adult | 200–400 mg/dL |
| Newborn | 125–300 mg/dL |
| Critical value | <100 mg/dL |
Increased platelet count (Thrombocytosis) may indicate:
- Iron deficiency anemia
- Malignant disorder
- Polycythemia vera
- Postsplenectomy syndrome
- Rheumatoid arthritis
Decreased platelet count (Thrombocytopenia) may indicate:
- Cancer
- Chemotherapy
- Disseminated intravascular coagulation
- Hemolytic anemia
- Hemorrhage
- Hypersplenism
- Immune thrombocytopenia
- Infection
- Inherited thrombocytopenia disorders such as Bernard-Soulier, Wiskott-Aldrich, or Zieve syndromes
- Leukemia and other myelofibrosis disorders
- Pernicious anemia
- Systemic lupus erythematosus
- Thrombotic thrombocytopenia
Nursing considerations for platelet count:
- High altitudes, persistent cold temperature, and strenuous exercise increase platelet counts.
- Assess the venipuncture site for bleeding in clients with known thrombocytopenia.
- Bleeding precautions should be instituted in clients with a low platelet count.
Bleeding Time Normal Lab Values
Bleeding time assess the overall hemostatic function (platelet response to injury and vasoconstrictive ability).
Indication for Bleeding Time
- Useful in detecting disorders of platelet function.
Prolonged bleeding time or increased levels may indicate:
- Bone marrow failure
- Bernard-Soulier syndrome
- Capillary fragility
- Clotting factor deficiency
- Collagen vascular disease
- Connective tissue disorder
- Cushing's syndrome
- Disseminated intravascular coagulation
- Glanzmann's thrombasthenia
- Henoch-Schonlein syndrome
- Hereditary telangiectasia
- Hypersplenism
- Leukemia
- Primary or metastatic tumor infiltration of bone marrow
- Severe liver disease
- Thrombocytopenia
- Uremia
- Von Willebrand's disease
Nursing Considerations for Bleeding Time
- Assess and validate that the client has not been receiving anticoagulants, aspirin, or aspirin-containing products for 3 days prior to the test.
- Inform the client that punctures are made to measure the time it takes for bleeding to stop.
- Apply pressure dressing to clients with bleeding tendencies after the procedure.
Normal Values for Bleeding Time
| Duke Method | Ivy Method |
|---|---|
| 1–3 minutes | 1–9 minutes |
D-Dimer Test
D-Dimer is a blood test that measures clot formation and lysis that results from the degradation of fibrin.
Indication of D-Dimer Test
- Helps to diagnose the presence of thrombus in conditions such as deep vein thrombosis, pulmonary embolism, or stroke.
- Used to diagnose disseminated intravascular coagulation (DIC).
- Monitor the effectiveness of treatment.
Normal Lab Value for D-Dimer:
| D-Dimer |
|---|
| <0.4 µg/mL |
Prothrombin Time, International Normalized Ratio (PT/INR)
Prothrombin is a vitamin K-dependent glycoprotein produced by the liver that is essential for fibrin clot formation. Each laboratory establishes a normal or control value based on the method used to perform the PT test. The PT measures the amount of time it takes in seconds for clot formation, the international normalized ratio (INR) is calculated from a PT result to monitor the effectiveness of warfarin.
Indication for PT and INR
- Monitor response to warfarin sodium (Coumadin) therapy.
- Screen for dysfunction of the extrinsic clotting system resulting from vitamin K deficiency disseminated intravascular coagulation or liver disease.
Normal and Critical Lab Values for Prothrombin Time (PT):
| Range | |
|---|---|
| Normal | 11—13 seconds |
| Full anticoagulant therapy | >1.5—2 times control value |
| Critical value | >20 seconds |
Normal and Critical Lab Value for International Normalized Ratio (INR)
The INR standardizes the PT ratio and is calculated in the laboratory setting by raising the observed PT ratio to the power of the international sensitivity index specific to the thromboplastin reagent used.
| Range | |
|---|---|
| Normal | 0.8—1.2 |
| Therapeutic INR range for patients on warfarin | 2.0—3.0 |
| Therapeutic INR range for patients with mechanical heart valves | 3.0—4.0 |
| Critical value | >5.0 |
Increased prothrombin time may indicate:
- Bile duct obstruction
- Coumarin ingestion
- Disseminated intravascular coagulation
- Hepatitis
- Hereditary factor deficiency
- Liver cirrhosis
- Massive blood transfusion
- Salicylate intoxication
- Vitamin K deficiency
Decreased prothrombin time may indicate:
- Blood clots quickly due to:
- Supplements containing vitamin K
- High intake of foods that contain vitamin K, such as liver, broccoli, kale, turnip greens and soybeans
Nursing Care for Prothrombin Time
- If a PT is prescribed, the baseline specimen should be drawn before anticoagulation therapy is started; note the time of collection on the laboratory form.
- Provide direct pressure to the venipuncture site for 3 to 5 minutes.
- Concurrent warfarin therapy with heparin therapy can lengthen the PT for up to 5 hours after dosing.
- Diets high in green leafy vegetables can increase the absorption of vitamin K, which shortens the PT.
- Orally administered anticoagulation therapy usually maintains the PT at 1.5 to 2 times the laboratory control value.
- Initiate bleeding precautions, if the PT value is longer than 30 seconds in a client receiving warfarin therapy.
Activated Partial Thromboplastin Time (APTT)
Activated partial thromboplastin time (APTT) evaluates the function of the contact activation pathway and coagulation sequence by measuring the amount of time it requires for recalcified citrated plasma to clot after partial thromboplastin is added to it. The test screens for deficiencies and inhibitors of all factors, except factors VII and XIII.
Normal and critical lab values for activated partial thromboplastin time (aPTT) and partial thromboplastin time (PTT):
| aPTT | PTT | |
|---|---|---|
| Normal | 30—40 seconds | 60—70 seconds |
| Patients receiving anticoagulant therapy | 1.5—2.5 times control value (60—80 seconds) | 1.5—2.5 seconds times control value (120—140 seconds) |
| Critical values | none or >70 seconds | none or >100 seconds |
Indication for APTT:
- Monitors the effectiveness of heparin therapy.
- Detect coagulation disorders in clotting factors such as hemophilia A (factor VIII) and hemophilia B (factor IX).
- Determine individuals who may be prone to bleeding during invasive procedures.
Increased APTT levels may indicate:
- Congenital clotting factor deficiencies
- Disseminated intravascular coagulation
- Hemophilia
- Heparin administration
- Hypofibrinogenemia von Willebrand's disease
- Leukemia
- Liver cirrhosis
- Vitamin K deficiency
Decreased APTT levels may indicate:
- Early stages of disseminated intravascular coagulation
- Extensive cancer
Nursing consideration for APTT:
- Do not draw samples from an arm into which heparin is infusing.
- If the client is receiving intermittent heparin by intermittent injection, plan to draw the blood sample 1 hour before the next dose of heparin.
- Apply direct pressure to the venipuncture site.
- Blood specimen should be transported to the laboratory immediately.
- The aPTT should be between 1.5 and 2.5 times normal when the client is receiving heparin therapy.
- Monitor for signs of bleeding if the aPTT value is longer than 90 seconds in a patient receiving heparin therapy.
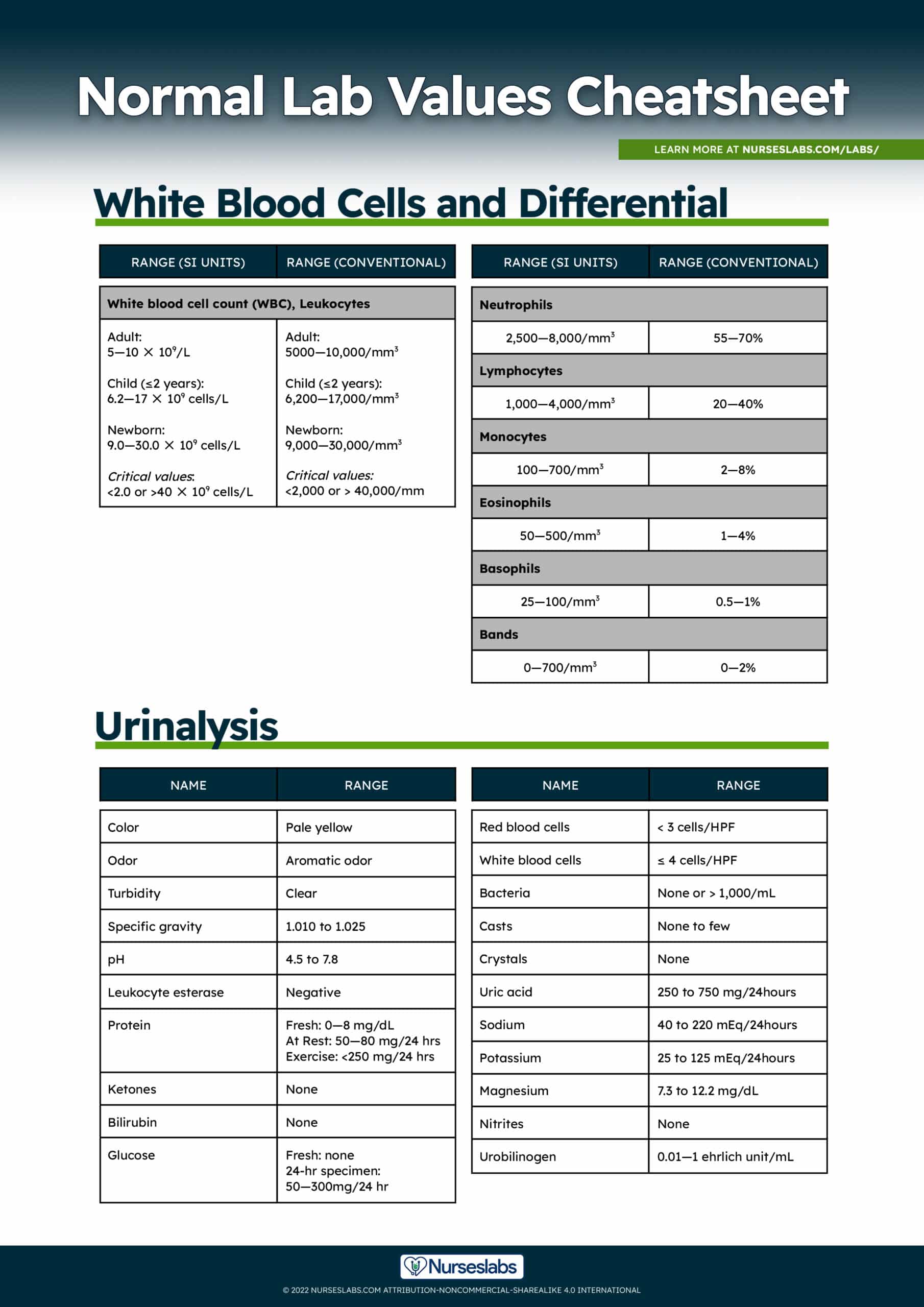
White Blood Cells and Differential
The normal laboratory value for WBC count has two components: the total number of white blood cells and differential count.
White Blood Cells (WBC)
White blood cells act as the body's first line of defense against foreign bodies, tissues, and other substances. WBC count assesses the total number of WBC in a cubic millimeter of blood. White blood cell differential provides specific information on white blood cell types:
- Neutrophils are the most common type of WBC and serve as the primary defense against infection.
- Lymphocytes play a big role in response to inflammation or infection.
- Monocytes are cells that respond to infection, inflammation, and foreign bodies by killing and digesting the foreign organism (phagocytosis).
- Eosinophils respond during an allergic reaction and parasitic infections.
- Basophils are involved during an allergic reaction, inflammation, and autoimmune diseases.
- Bands are immature WBCs that are first released from the bone marrow into the blood.
Normal and critical lab values for white blood cell count:
| Range (SI Units) | Range (Conventional) | |
|---|---|---|
| Adult | 5.0—10 ✕ 109 cells/L | 5000—10,000/mm3 |
| Child (≤2 years) | 6.2—17 ✕ 109 cells/L | 6,200—17,000/mm3 |
| Newborn | 9.0—30 ✕ 109 cells/L | 9,000—30,000/mm3 |
| Critical values | 2.0—40 ✕ 109 cells/L | <2,000 or > 40,000/mm |
Normal lab values for WBC differential:
| WBC | Range (SI Unit) | Range (Conventional) |
|---|---|---|
| Neutrophils | 2,500—8,000/mm3 | 55—70% |
| Lymphocytes | 1,000—4,000/mm3 | 20—40% |
| Monocytes | 100—700/mm3 | 2—8% |
| Eosinophils | 50—500/mm3 | 1—4% |
| Basophils | 25—100/mm3 | 0.5—1% |
| Bands | 0—700/mm3 | 0—2% |
Increased WBC count (Leukocytosis) may indicate:
- Inflammation
- Infection
- Leukemic neoplasia
- Stress
- Tissue necrosis
- Trauma
Decreased WBC count (Leukopenia) may indicate:
- Autoimmune disease
- Bone marrow failure
- Bone marrow infiltration (e.g., myelofibrosis)
- Congenital marrow aplasia
- Drug toxicity (e.g., chloramphenicol)
- Nutritional deficiency
- Severe infection
Nursing consideration for WBC count:
- A high total WBC count with a left shift means that the bone marrow will release an increased amount of neutrophils in response to inflammation or infection.
- A "shift to the right" which is usually seen in liver disease, megaloblastic and pernicious anemia, and Down syndrome, indicates that cells have more than the usual number of nuclear segments.
- A "shift to the left" indicates an increased number of immature neutrophils is found in the blood.
- A low total WBC count with a left shift means a recovery from bone marrow depression or an infection of such intensity that the demand for neutrophils in the tissue is greater than the capacity of the bone marrow to release them into the circulation.
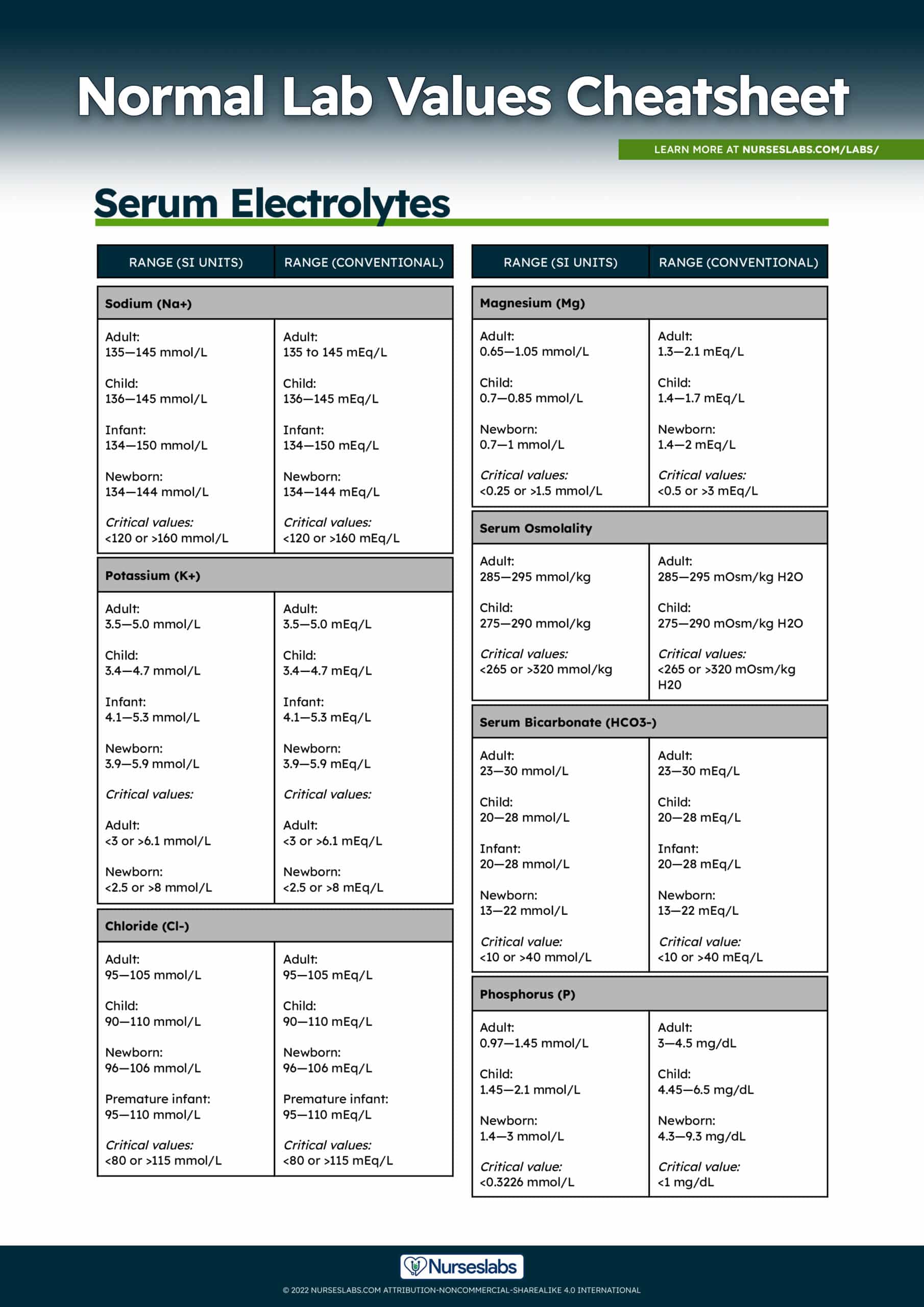
Serum Electrolytes Normal Lab Values
Electrolytes are minerals that are involved in some of the important functions in our body. Serum electrolytes are routinely ordered for a patient admitted to a hospital as a screening test for electrolyte and acid-base imbalances. Here we discuss the normal lab values of the commonly ordered serum tests: potassium, serum sodium, serum chloride, and serum bicarbonate. Serum electrolytes may be ordered as a "Chem 7" or as a "basic metabolic panel (BMP)".
Serum Sodium (Na+) Normal Lab Values
Sodium is a major cation of extracellular fluid that maintains osmotic pressure and acid-base balance, and assists in the transmission of nerve impulses. Sodium is absorbed from the small intestine and excreted in the urine in amounts dependent on dietary intake.
Normal and critical values for serum Sodium (Na+):
| Range (SI Units) | Range (Conventional) | |
|---|---|---|
| Adult | 135—145 mmol/L | 135—145 mEq/L |
| Child | 136—145 mmol/L | 136—145 mEq/L |
| Infant | 134—150 mmol/L | 134—150 mEq/L |
| Newborn | 134—144 mmol/L | 134—144 mEq/L |
| Critical values | <120 or >160 mmol/L | <120 or >160 mEq/L |
Indications for Serum Sodium
- Determine whole-body stores of sodium, because the ion is predominantly extracellular
- Monitor the effectiveness of drug, especially diuretics, on serum sodium levels.
Increased sodium levels (Hypernatremia) may indicate:
- Cushing's syndrome
- Diabetes insipidus
- Excessive dietary intake
- Excessive IV sodium administration
- Excessive sweating
- Extensive thermal burns
- Hyperaldosteronism
- Osmotic diuresis
Decreased sodium levels (Hyponatremia) may indicate:
- Ascites
- Addison's disease
- Congestive heart failure
- Chronic renal insufficiency
- Deficient dietary intake
- Deficient sodium in IV fluids
- Diarrhea
- Diuretic administration
- Excessive oral water intake
- Excessive IV water intake
- Intraluminal bowel loss (e.g., ileus or mechanical obstruction)
- Osmotic dilution
- Peripheral edema
- Pleural effusion
- Syndrome of inappropriate ADH (SIADH) secretion
- Vomiting or nasogastric aspiration
Nursing consideration for Serum Sodium
- Drawing blood samples from an extremity in which an intravenous (IV) solution of sodium chloride is infusing increases the level, producing inaccurate results.
Serum Potassium (K+)
Potassium is the most abundant intracellular cation that serves important functions such as regulate acid-base equilibrium, control cellular water balance, and transmit electrical impulses in skeletal and cardiac muscles.
Normal and critical values for Potassium (K+):
| Range (SI Units) | Range (Conventional) | |
|---|---|---|
| Adult | 3.5—5.0 mmol/L | 3.5—5.0 mEq/L |
| Child | 3.4—4.7 mmol/L | 3.4—4.7 mEq/L |
| Infant | 4.1—5.3 mmol/L | 4.1—5.3 mEq/L |
| Newborn | 3.9—5.9 mmol/L | 3.9—5.9 mEq/L |
| Critical values (Adult) | <3.0 or >6.1 mmol/L | <3.0 or >6.1 mEq/L |
| Critical values (Newborn) | <2.5 or >8.0 mmol/L | <2.5 or >8.0 mEq/L |
Indications for Serum Potassium
- Evaluates cardiac function, renal function, gastrointestinal function, and the need for IV replacement therapy.
Increased potassium levels (Hyperkalemia) may indicate:
- Acidosis
- Acute or chronic renal failure
- Aldosterone-inhibiting diuretics
- Crush injuries to tissues
- Dehydration
- Excessive dietary intake
- Excessive IV intake
- Hemolysis
- Hemolyzed blood transfusion
- Hypoaldosteronism
- Infection
Decreased potassium levels (Hypokalemia) may indicate:
- Ascites
- Burns
- Cushing's syndrome
- Cystic fibrosis
- Deficient dietary intake
- Deficient IV intake
- Diuretics
- Gastrointestinal disorders such as nausea and vomiting
- Glucose administration
- Hyperaldosteronism
- Insulin administration
- Licorice administration
- Renal artery stenosis
- Renal tubular acidosis
- Surgery
- Trauma
Nursing Considerations for Serum Potassium
- Note on the laboratory form if the client is receiving potassium supplementation.
- Clients with elevated white blood cell counts and platelet counts may have falsely elevated potassium levels.
Serum Chloride (Cl-)
Chloride is a hydrochloric acid salt that is the most abundant body anion in the extracellular fluid. Functions to counterbalance cations, such as sodium, and acts as a buffer during oxygen and carbon dioxide exchange in red blood cells (RBCs). Aids in digestion and maintaining osmotic pressure and water balance.
Normal and critical values for Chloride (Cl-):
| Range (SI Units) | Range (Conventional) | |
|---|---|---|
| Adult | 95—105 mmol/L | 95—105 mEq/L |
| Child | 90—110 mmol/L | 90—110 mEq/L |
| Newborn | 96—106 mmol/L | 96—106 mEq/L |
| Premature infant | 95—110 mmol/L | 95—110 mEq/L |
| Critical values | <80 or >115 mmol/L | <80 or >115 mEq/L |
Increased chloride levels (Hyperchloremia) may indicate:
- Anemia
- Cushing's syndrome
- Dehydration
- Eclampsia
- Excessive infusion of normal saline
- Hyperparathyroidism
- Hyperventilation
- Kidney dysfunction
- Metabolic acidosis
- Multiple myelomas
- Renal tubular acidosis
- Respiratory alkalosis
Decreased chloride levels (Hypochloremia) may indicate:
- Addison's disease
- Aldosteronism
- Burns
- Chronic gastric suction
- Chronic respiratory acidosis
- Congestive heart failure
- Diuretic therapy
- Hypokalemia
- Metabolic alkalosis
- Overhydration
- Respiratory alkalosis
- Salt-losing nephritis
- Syndrome of inappropriate antidiuretic hormone (SIADH)
- Vomiting
Nursing Considerations for Serum Chloride
- Any condition accompanied by prolonged vomiting, diarrhea, or both will alter chloride levels.
Magnesium (Mg)
Magnesium is used as an index to determine metabolic activity and renal function. Magnesium is needed in the blood-clotting mechanisms, regulates neuromuscular activity, acts as a cofactor that modifies the activity of many enzymes, and has an effect on the metabolism of calcium.
Normal and critical values for Magnesium (Mg):
| Range (SI Units) | Range (Conventional) | |
|---|---|---|
| Adult | 0.7—1.05 mmol/L | 1.3—2.1 mEq/L |
| Child | 0.7—0.85 mmol/L | 1.4—1.7 mEq/L |
| Newborn | 0.7—1.0 mmol/L | 1.4—2.0 mEq/L |
| Critical values | <0.25 or >1.5 mmol/L | <0.5 or >3.0 mEq/L |
Increased magnesium levels (Hypermagnesemia) may indicate:
- Addison's disease
- Hypothyroidism
- Ingestion of magnesium-containing antacids or salt
- Renal insufficiency
- Uncontrolled diabetes
Decreased magnesium levels (Hypomagnesemia) may indicate:
- Alcoholism
- Chronic renal disease
- Diabetic acidosis
- Hypoparathyroidism
- Malabsorption
- Malnutrition
Nursing Considerations
- Prolonged use of magnesium products causes increased serum levels.
- Long-term parenteral nutrition therapy or excessive loss of body fluids may decrease serum levels.
Serum Osmolality
Serum osmolality is a measure of the solute concentration of the blood. Particles include sodium ions, glucose, and urea. Serum osmolality is usually estimated by doubling the serum sodium because sodium is a major determinant of serum osmolality.
Normal and critical values for Serum Osmolality:
| Range (SI Units) | Range (Conventional) | |
|---|---|---|
| Adult | 285—295 mmol/kg | 285—295 mOsm/kg H2O |
| Child | 275—290 mmol/kg | 275—290 mOsm/kg H2O |
| Critical values | <265 or >320 mmol/kg | <265 or >320 mOsm/kg H20 |
Serum Bicarbonate (HCO3-)
Part of the bicarbonate-carbonic acid buffering system and mainly responsible for regulating the pH of body fluids.
Normal and critical values for Serum Bicarbonate (HCO3-):
| Range (SI Units) | Range (Conventional) | |
|---|---|---|
| Adult | 23—30 mmol/L | 23—30 mEq/L |
| Child | 20—28 mmol/L | 20—28 mEq/L |
| Infant | 20—28 mmol/L | 20—28 mEq/L |
| Newborn | 13—22 mmol/L | 13—22 mEq/L |
| Critical values | <10 or >40 mmol/L | <10 or >40 mEq/L |
Nursing consideration for Serum Bicarbonate
- Ingestion of acidic or alkaline solutions may cause increased or decreased results, respectively.
Phosphorus (P)
Phosphorus (Phosphate) is important in bone formation, energy storage and release, urinary acid-base buffering, and carbohydrate metabolism. Phosphorus is absorbed from food and is excreted by the kidneys. High concentrations of phosphorus are stored in bone and skeletal muscle.
Normal and critical values for Phosphorus (P):
| Range (SI Units) | Range (Conventional) | |
|---|---|---|
| Adult | 0.97—1.45 mmol/L | 3.0—4.5 mg/dL |
| Child | 1.45—2.1 mmol/L | 4.45—6.5 mg/dL |
| Newborn | 1.4—3.0 mmol/L | 4.3—9.3 mg/dL |
| Critical values | <0.32 mmol/L | <1.0 mg/dL |
Increased phosphorus levels (Hyperphosphatemia) may indicate:
- Acidosis
- Acromegaly
- Advanced myeloma or lymphoma
- Bone metastasis
- Hemolytic anemia
- Hypocalcemia
- Hypoparathyroidism
- Increased dietary or IV intake of phosphorus
- Liver disease
- Renal failure
- Rhabdomyolysis
- Sarcoidosis
Decreased phosphorus levels (Hypophosphatemia) may indicate:
- Alkalosis
- Chronic alcoholism
- Chronic antacid ingestion
- Diabetic acidosis
- Hypercalcemia
- Hyperinsulinism
- Hyperparathyroidism
- Inadequate dietary ingestion of phosphorus
- Malnutrition
- Osteomalacia (adult)
- Rickets (child)
- Sepsis
- Vitamin D deficiency
Nursing Consideration
- Instruct the client to fast before the test.
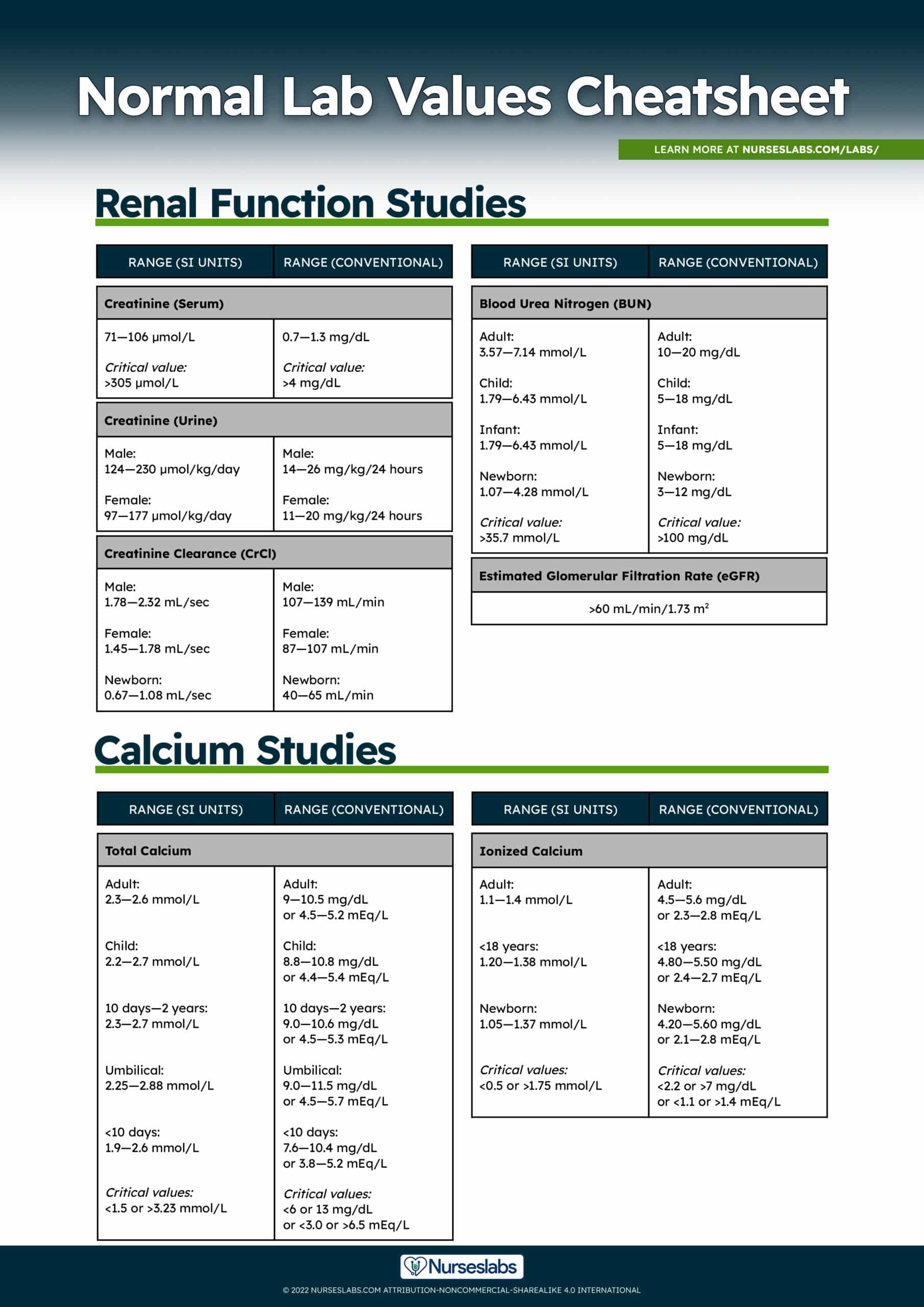
Total Calcium (Ca+), Ionized Calcium
Calcium (Ca+) is a cation absorbed into the bloodstream from dietary sources and functions in bone formation, nerve impulse transmission, and contraction of myocardial and skeletal muscles. Calcium aids in blood clotting by converting prothrombin to thrombin.
Normal and critical values for Total Calcium (Ca):
| Range (SI Units) | Range (Conventional) | |
|---|---|---|
| Adult | 2.3—2.6 mmol/L | 9.0—10.5 mg/dL or 4.5—5.2 mEq/L |
| Child | 2.2—2.7 mmol/L | 8.8—10.8 mg/dL or 4.4—5.4 mEq/L |
| 10 days to 2 years | 2.3—2.7 mmol/L | 9.0—10.6 mg/dL or 4.5—5.3 mEq/L |
| Umbilical | 2.3—2.9 mmol/L | 9.0—11.5 mg/dL or 4.5—5.7 mEq/L |
| <10 days | 1.9—2.6 mmol/L | 7.6—10.4 mg/dL or 3.8—5.2 mEq/L |
| Critical values | <1.5 or >3.2 mmol/L | <6.0 or 13 mg/dL or <3.0 or >6.5 mEq/L |
Normal and critical values for Ionized Calcium:
| Range (SI Units) | Range (Conventional) | |
|---|---|---|
| Adult | 1.1—1.4 mmol/L | 4.5—5.6 mg/dL or 2.3—2.8 mEq/L |
| <18 years | 1.2—1.4 mmol/L | 4.8—5.5 mg/dL or 2.4—2.7 mEq/L |
| Newborn | 1.1—1.4 mmol/L | 4.2—5.6 mg/dL or 2.1—2.8 mEq/L |
| Critical values | <0.5 or >1.8 mmol/L | <2.2 or >7.0 mg/dL or <1.1 or >1.4 mEq/L |
Increased calcium levels (Hypercalcemia) may indicate:
- Acromegaly
- Addison's disease
- Granulomatous infections such as tuberculosis and sarcoidosis
- Hyperparathyroidism
- Hyperthyroidism
- Lymphoma
- Metastatic tumor to the bone
- Milk-alkali syndrome
- Nonparathyroid PTH-producing tumor such as renal or lung carcinoma
- Paget's disease of bone
- Prolonged immobilization
- Vitamin D intoxication
Decreased calcium levels (Hypocalcemia) may indicate:
- Alkalosis
- Fat embolism
- Hyperphosphatemia secondary to renal failure
- Hypoparathyroidism
- Malabsorption
- Osteomalacia
- Pancreatitis
- Renal failure
- Rickets
- Vitamin D deficiency
Nursing Considerations
- Instruct the client to eat a diet with a normal calcium level (800 mg/day) for 3 days before the exam.
- Instruct the client that fasting may be required for 8 hours before the test.
- Note that calcium levels can be affected by decreased protein levels and the use of anticonvulsant medications
Renal Function Studies Normal Lab Values
In this section, we'll be discussing the normal laboratory values of serum creatinine and blood urea nitrogen, including their indications and nursing considerations. These laboratory tests are helpful in determining the kidney function of an individual.
Serum Creatinine (Cr), Creatinine (Urine), and Creatinine Clearance (CrCl)
Creatinine is a specific indicator of renal function. Increased levels of creatinine indicate a slowing of the glomerular filtration rate.
Normal and critical values for Creatinine (Serum):
| Range (SI Units) | Range (Conventional) | |
|---|---|---|
| Creatinine (Serum) | 285—295 mmol/kg | 285—295 mOsm/kg H2O |
| Critical values | 275—290 mmol/kg | 275—290 mOsm/kg H2O |
Normal values for Creatinine (Urine):
| Range (SI Units) | Range (Conventional) | |
|---|---|---|
| Male | 124—230 µmol/kg/day | 14—26 mg/kg/24 hours |
| Female | 97—177 µmol/kg/day | 11—20 mg/kg/24 hours |
Normal lab values for Creatinine Clearance (CrCl):
| Range (SI Units) | Range (Conventional) | |
|---|---|---|
| Male | 1.78—2.32 mL/sec | 107—139 mL/min |
| Female | 1.45—1.78 mL/sec | 87—107 mL/min |
| Newborn | 0.67—1.08 mL/sec | 40—65 mL/min |
Increased creatinine levels may indicate:
- Acromegaly
- Acute tubular necrosis
- Congestive heart failure
- Dehydration
- Diabetic nephropathy
- Gigantism
- Glomerulonephritis
- Nephritis
- Pyelonephritis
- Rhabdomyolysis
- Shock
- Urinary tract obstruction
Decreased creatinine levels may indicate:
- Debilitation
- Myasthenia gravis
- Muscular dystrophy
Nursing Considerations
- Instruct the client to avoid excessive exercise for 8 hours and excessive red meat intake for 24 hours before the test.
Blood Urea Nitrogen (BUN)
Urea nitrogen is the nitrogen portion of urea, a substance formed in the liver through an enzymatic protein breakdown process. Urea is normally freely filtered through the renal glomeruli, with a small amount reabsorbed in the tubules and the remainder excreted in the urine. Elevated levels indicate a slowing of the glomerular filtration rate.
Normal lab values and critical values for Blood Urea Nitrogen (BUN):
| Range (SI Units) | Range (Conventional) | |
|---|---|---|
| Adult | 3.57—7.14 mmol/L | 10—20 mg/dL |
| Child | 1.79—6.43 mmol/L | 5—18 mg/dL |
| Infant | 1.79—6.43 mmol/L | 5—18 mg/dL |
| Newborn | 1.07—4.28 mmol/L | 3—12 mg/dL |
| Critical values | >35.7 mmol/L | >100 mg/dL |
Normal value for Estimate Glomerular Filtration Rate (eGFR):
| Estimated Glomerular Filtration Rate (eGFR) |
|---|
| >60 mL/min/1.73 m2 |
Increased blood urea nitrogen levels may indicate:
- Alimentary tube feeding
- Bladder outlet obstructions
- Burns
- Congestive heart failure
- Dehydration
- Excessive protein catabolism
- Excessive protein ingestion
- Gastrointestinal (GI) bleeding
- Glomerulonephritis
- Hypovolemia
- Myocardial infarction
- Nephrotoxic drugs
- Pyelonephritis
- Renal failure
- Sepsis
- Shock
- Starvation
- Ureteral obstruction
Decreased blood urea nitrogen levels may indicate:
- Liver failure
- Malnutrition or malabsorption
- Nephrotic syndrome
- Overhydration due to fluid overload or syndrome of inappropriate antidiuretic hormone (SIADH)
- Pregnancy
Nursing consideration
- BUN and creatinine ratios should be analyzed when renal function is evaluated.
Liver Function Studies Normal Lab Values
Conditions affecting the gastrointestinal tract can be easily evaluated by studying the normal laboratory values of alanine aminotransferase, aspartate aminotransferase, bilirubin, albumin, ammonia, amylase, lipase, protein, and lipids.
Alanine Aminotransferase (ALT)
Alanine Aminotransferase (ALT) test is used to identify hepatocellular injury and inflammation of the liver and to monitor improvement or worsening of the disease. ALT was formerly known as serum pyretic transaminase (SGPT).
Normal values for Alanine Aminotransferase (ALT, SGPT):
| Range (SI Units) | Range (Conventional) | |
|---|---|---|
| Male | 0.17—0.92 µkat/L | 10—55 units/L |
| Female | 0.12—0.50 µkat/L | 7—30 units/L |
Increased Alanine Aminotransferase (ALT)
Levels may indicate:
- Cirrhosis
- Cholestasis
- Hepatitis
- Hepatic ischemia
- Hepatic necrosis
- Hepatic tumor
- Hepatotoxic drugs
- Infectious mononucleosis
- Myocardial infarction
- Myositis
- Obstructive jaundice
- Pancreatitis
- Severe burns
- Shock
- Trauma to striated muscle
Decreased Alanine Aminotransferase (ALT) levels:
- Is expected and is normal
Nursing Considerations
- No fasting is required.
- Previous intramuscular injections may cause elevated levels.
Aspartate Aminotransferase (AST)
Aspartate Aminotransferase (AST) test is used to evaluate a client with a suspected hepatocellular disease, injury, or inflammation (may also be used along with cardiac markers to evaluate coronary artery occlusive disease). AST was formerly known as serum glutamic-oxaloacetic transaminase (SGOT).
Normal values for Aspartate Aminotransferase (AST, SGOT):
| Range (SI Units) | Range (Conventional) | |
|---|---|---|
| Male | 0.17—0.67 µkat/L | 10—40 units/L |
| Female | 0.15—0.42 µkat/L | 9—25 units/L |
Increased Aspartate Aminotransferase (AST) levels may indicate:
- Heart diseases
- Cardiac operations
- Cardiac catheterization and angioplasty
- Myocardial infarctions
- Liver diseases
- Drug-induced liver injury
- Hepatitis
- Hepatic cirrhosis
- Hepatic infiltrative process
- Hepatic metastasis
- Hepatic necrosis
- Hepatic surgery
- Infectious mononucleosis with hepatitis
- Skeletal muscle diseases
- Heat stroke
- Multiple traumas
- Primary muscle diseases
- Progressive muscular dystrophy
- Recent convulsions
- Recent noncardiac surgery
- Severe, deep burns
- Skeletal muscle trauma
- Other diseases
- Acute hemolytic anemia
- Acute pancreatitis
Decreased Aspartate Aminotransferase (AST) levels may indicate:
- Acute renal disease
- Beriberi
- Chronic renal dialysis
- Diabetic ketoacidosis
- Pregnancy
Nursing Considerations
- No fasting is required.
- Previous intramuscular injections may cause elevated levels.
Bilirubin
Bilirubin is produced by the liver, spleen, and bone marrow and is also a by-product of hemoglobin breakdown. Total bilirubin levels can be broken into direct bilirubin, which is excreted primarily via the intestinal tract, and indirect bilirubin, which circulates primarily in the bloodstream. Total bilirubin levels increase with any type of jaundice; direct and indirect bilirubin levels help differentiate the cause of jaundice.
Normal values and critical values for total, direct, and indirect bilirubin:
| Range (SI Units) | Range (Conventional) | |
|---|---|---|
| Adult | 5.1—17 μmol/L | 0.3—1.0 mg/dL |
| Newborn | 17.1—205 µmol/L | 1.0—12.0 mg/dL |
| Critical values (Adult) | >205 µmol/L | >12 mg/dL |
| Critical values (Newborn) | >256 µmol/L | >15 mg/dL |
| Direct bilirubin (conjugated) | 1.7—5.1 μmol/L | 0.1—0.3 mg/dL |
| Indirect bilirubin (unconjugated) | 3.4—12.0 μmol/L | 0.2—0.8 mg/dL |
Increased conjugated (direct) bilirubin levels may indicate:
- Cholestasis from drugs
- Dubin-Johnson syndrome
- Extensive liver metastasis
- Extrahepatic duct obstruction (gallstone, inflammation, scarring, surgical trauma, or tumor)
- Gallstones
- Rotor's syndrome
Increased unconjugated (indirect) bilirubin levels may indicate:
- Cirrhosis
- Crigler-Najjar syndrome
- Erythroblastosis fetalis
- Gilbert's syndrome
- Hemolytic anemia
- Hemolytic jaundice
- Hepatitis
- Large-volume blood transfusion
- Neonatal hyperbilirubinemia
- Resolution of a large hematoma
- Pernicious anemia
- Sepsis
- Sickle cell anemia
- Transfusion reaction
Nursing Considerations
- Instruct the client to eat a diet low in yellow foods, avoiding foods such as carrots, yams, yellow beans, and pumpkin, for 3 to 4 days before the blood is drawn.
- Instruct the client to fast for 4 hours before the blood is drawn.
- Note that results will be elevated with the ingestion of alcohol or the administration of morphine sulfate, theophylline, ascorbic acid (vitamin C), or acetylsalicylic acid (Aspirin).
- Note that results are invalidated if the client has received a radioactive scan within 24 hours before the test.
Albumin
Albumin is the main plasma protein of blood that maintains oncotic pressure and transports bilirubin, fatty acids, medications, hormones, and other substances that are insoluble in water. Albumin is increased in conditions such as dehydration, diarrhea, and metastatic carcinoma; decreased in conditions such as acute infection, ascites, and alcoholism. Presence of detectable albumin, or protein, in the urine is indicative of abnormal renal function.
Normal lab values for Albumin:
| Range (SI Units) | Range (Conventional) | |
|---|---|---|
| Adult | 35—50 g/L | 3.5—5.0 g/dL |
| Child | 40—59 g/L | 4.0—5.9 g/dL |
| Infant | 44—54 g/L | 4.4—5.4 g/dL |
| Newborn | 35—54 g/L | 3.5—5.4 g/dL |
| Premature infant | 30—42 g/L | 3.0—4.2 g/dL |
Increased albumin levels (Hyperalbuminemia) may indicate:
- Dehydration
- Severe diarrhea
- Severe vomiting
Decreased albumin levels (Hypoalbuminemia) may indicate:
- Acute liver failure
- Cirrhosis
- Familial idiopathic dysproteinemia
- Inflammatory disease
- Increased capillary permeability
- Malnutrition
- Pregnancy
- Protein-losing enteropathies
- Protein-losing nephropathies
- Severe burns
- Severe malnutrition
- Ulcerative colitis
Nursing Considerations
- Fasting is not required.
Ammonia
Ammonia is a by-product of protein catabolism; most of it is created by bacteria acting on proteins present in the gut. Ammonia is metabolized by the liver and excreted by the kidneys as urea. Elevated levels resulting from hepatic dysfunction may lead to encephalopathy. Venous ammonia levels are not a reliable indicator of hepatic coma.
Normal values for Ammonia:
| Range (SI Units) | Range (Conventional) | |
|---|---|---|
| Adult | 7—57 µmol/L | 10—80 µg/dL |
| Child | 29—57 µmol/L | 40—80 µg/dL |
| Newborn | 64—107 µmol/L | 90—150 µg/dL |
Nursing Considerations
- Instruct the client to fast, except for water, and to refrain from smoking for 8 to 10 hours before the test; smoking increases ammonia levels.
- Place the specimen on ice and transport to the laboratory immediately.
Amylase
Amylase is an enzyme, produced by the pancreas and salivary glands, aids in the digestion of complex carbohydrates and is excreted by the kidneys. In acute pancreatitis, the amylase level may exceed five times the normal value; the level starts rising 6 hours after the onset of pain, peaks at about 24 hours, and returns to normal in 2 to 3 days after the onset of pain. In chronic pancreatitis, the rise in serum amylase usually does not normally exceed three times the normal value.
Normal values for amylase:
| Range (SI Units) | Range (Conventional) | |
|---|---|---|
| Adult | 30–220 units/L or 500 nkat/L | 60—120 Somogyi units/dL |
| Newborn | 3—32.5 units/L or 50—542 nkat/L | 6—65 Somogyi units/dL |
Increased amylase levels may indicate:
- Acute pancreatitis
- Acute cholecystitis
- Diabetic ketoacidosis
- Duodenal obstruction
- Ectopic pregnancy
- Necrotic bowel
- Parotiditis
- Penetrating peptic ulcer
- Perforated peptic ulcer
- Perforated bowel
- Pulmonary infarction
Decreased amylase levels may indicate:
- Chronic pancreatitis
- Cystic fibrosis
- Liver disease
- Preeclampsia
Nursing Considerations
- On the laboratory form, list the medications that the client has taken during the previous 24 hours before the test.
- Note that many medications may cause false-positive or false-negative results.
- Results are invalidated if the specimen was obtained less than 72 hours after cholecystography with radiopaque dyes.
Lipase
Lipase is a pancreatic enzyme converts fats and triglycerides into fatty acids and glycerol. Elevated lipase levels occur in pancreatic disorders; elevations may not occur until 24 to 36 hours after the onset of illness and may remain elevated for up to 14 days.
Normal values for Lipase:
| Lipase |
|---|
| 0—160 units/L |
Increased lipase levels may indicate:
- Acute cholecystitis
- Acute pancreatitis
- Bowel obstruction or infarction
- Cholangitis
- Chronic relapsing pancreatitis
- Extrahepatic duct obstruction
- Pancreatic cancer
- Pancreatic pseudocyst
- Peptic ulcer disease
- Renal failure
- Salivary gland inflammation or tumor
Decreased lipase levels may indicate:
- Chronic conditions such as cystic fibrosis
Nursing Consideration
- Endoscopic retrograde cholangiopancreatography (ERCP) may increase lipase activity.
Serum Protein
Serum protein reflects the total amount of albumin and globulins in the plasma. Protein regulates osmotic pressure and is necessary for the formation of many hormones, enzymes, and antibodies; it is a major source of building material for blood, skin, hair, nails, and internal organs. Increased in conditions such as Addison's disease, autoimmune collagen disorders, chronic infection, and Crohn's disease. Decreased in conditions such as burns, cirrhosis, edema, and severe hepatic disease.
Normal values for Total Protein (Serum):
| Range (SI Units) | Range (Conventional) | |
|---|---|---|
| Adult | 54—83 g/L | 5.4—8.3 g/dL |
| Child | 62—80 g/L | 6.2—8.0 g/dL |
| Infant | 60—67 g/L | 6.0—6.7 g/dL |
| Newborn | 46—74 g/L | 4.6—7.4 g/dL |
| Premature infant | 42—76 g/L | 4.2—7.6 g/dL |
Increased protein levels may indicate:
- Amyloidosis
- Dehydration
- Hepatitis B
- Hepatitis C
- Human immunodeficiency virus
- Multiple myeloma
Decreased protein levels may indicate:
- Agammaglobulinemia
- Bleeding
- Celiac disease
- Extensive burns
- Inflammatory bowel disease
- Kidney disorder
- Liver disease
- Severe malnutrition
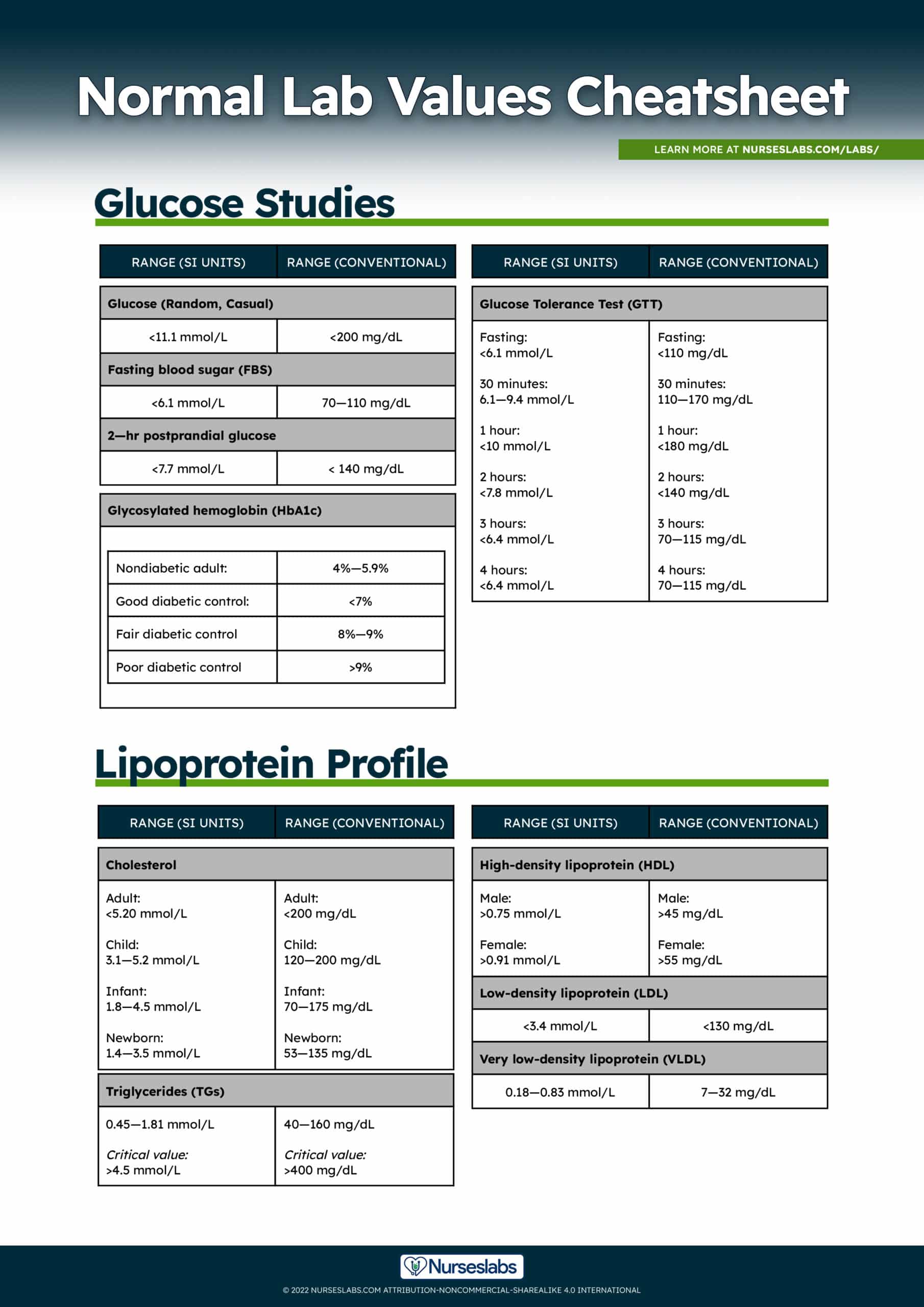
Glucose Studies Normal Lab Values
Understanding the normal laboratory values of blood glucose is an essential key in managing diabetes mellitus. Included in this section are the lab values and nursing considerations for glycosylated hemoglobin, fasting blood sugar, glucose tolerance test, and diabetes mellitus antibody panel.
Fasting Blood Glucose
Fasting blood glucose or fasting blood sugar (FBS) levels are used to help diagnose diabetes mellitus and hypoglycemia. Glucose is a monosaccharide found in fruits and is formed from the digestion of carbohydrates and the conversion of glycogen by the liver. Glucose is the main source of cellular energy for the body and is essential for brain and erythrocyte function.
Normal values for Glucose Studies:
| Range (SI Units) | Range (Conventional) | |
|---|---|---|
| Glucose (Random, Casual) | <11.1 mmol/L | <200 mg/dL |
| Fasting Blood Sugar (FBS) | <6.1 mmol/L | 70—110 mg/dL |
| 2-hr Postprandial Glucose | <7.7 mmol/L | < 140 mg/dL |
Increased glucose levels (Hyperglycemia) may indicate:
- Acromegaly
- Acute pancreatitis
- Acute stress response
- Chronic renal failure
- Corticosteroid therapy
- Cushing's syndrome
- Diabetes mellitus
- Diuretic therapy
- Glucagonoma
- Pheochromocytoma
Increased postprandial glucose levels (Postprandial hyperglycemia) may indicate:
- Acromegaly
- Acute stress response
- Chronic renal failure
- Corticosteroid therapy
- Cushing's syndrome
- Diabetes mellitus
- Diuretic therapy
- Extensive liver disease
- Gestational diabetes mellitus
- Glucagonoma
- Hyperthyroidism
- Malnutrition
- Pheochromocytoma
Decreased glucose levels (Hypoglycemia) may indicate:
- Addison's disease
- Extensive liver disease
- Hypopituitarism
- Hypothyroidism
- Insulinoma
- Insulin overdose
- Starvation
Decreased postprandial glucose levels (Postprandial hypoglycemia) may indicate:
- Addison's disease
- Hypopituitarism
- Hypothyroidism
- Insulinoma
- Insulin overdose
- Malabsorption or maldigestion
Nursing consideration:
- Instruct the client to fast for 8 to 12 hours before the test.
- Instruct a client with diabetes mellitus to withhold morning insulin or oral hypoglycemic medication until after the blood is drawn.
Glucose Tolerance Test (GTT)
The glucose tolerance test (GTT) aids in the diagnosis of diabetes mellitus. If the glucose levels peak at higher than normal at 1 and 2 hours after injection or ingestion of glucose and are slower than normal to return to fasting levels, then diabetes mellitus is confirmed.
Normal values for Glucose Tolerance Test (GTT):
| Range (SI Units) | Range (Conventional) | |
|---|---|---|
| Fasting | <6.1 mmol/L | <110 mg/dL |
| 30 minutes | 6.1—9.4 mmol/L | 110—170 mg/dL |
| 1 hour | <10.0 mmol/L | <180 mg/dL |
| 2 hours | <7.8 mmol/L | <140 mg/dL |
| 3 hours | <6.4 mmol/L | 70—115 mg/dL |
| 4 hours | <6.4 mmol/L | 70—115 mg/dL |
Abnormal Glucose tolerance test may indicate:
- Acromegaly
- Acute pancreatitis
- Acute stress response
- Chronic renal failure
- Corticosteroid therapy
- Cushing's syndrome
- Diabetes mellitus
- Diuretic therapy
- Glucagonoma
- Myxedema
- Pheochromocytoma
- Post-gastrectomy
- Somogyi response to hypoglycemia
Nursing Considerations
- Instruct the client to eat a high-carbohydrate (200 to 300 g) diet for 3 days before the test.
- Instruct the client to avoid alcohol, coffee, and smoking for 36 hours before the test.
- Instruct the client to avoid strenuous exercise for 8 hours before and after the test.
- Instruct the client to fast for 10 to 16 hours before the test.
- Instruct the client with diabetes mellitus to withhold morning insulin or oral hypoglycemic medication.
- Instruct the client that the test may take 3 to 5 hours, requires IV or oral administration of glucose, and the taking of multiple blood samples.
Glycosylated Hemoglobin (HbA1c)
Glycosylated hemoglobin is blood glucose bound to hemoglobin. Hemoglobin A₁C (glycosylated hemoglobin A; HbA1c) is a reflection of how well blood glucose levels have been controlled for the past 3 to 4 months. Hyperglycemia in clients with diabetes is usually a cause of an increase in the HbA1c.
Reference values for Glycosylated hemoglobin (HbA1c):
| Range | |
|---|---|
| Nondiabetic adult | 4%—5.9% |
| Good diabetic control | <7% |
| Fair diabetic control | 8%—9% |
| Poor diabetic control | >9% |
Increased Glycosylated hemoglobin (HbA1c) levels may indicate:
- Newly diagnosed diabetic patient
- Non-diabetic hyperglycemia
- Poorly controlled diabetic patient
- Pregnancy
- Splenectomized patients
Decreased Glycosylated hemoglobin (HbA1c) levels may indicate:
- Chronic blood loss
- Chronic renal failure
- Hemolytic anemia
Nursing Consideration
- Fasting is not required before the test.
Diabetes Mellitus Autoantibody Panel
Used to evaluate insulin resistance and to identify type 1 diabetes and clients with a suspected allergy to insulin.
Normal Lab Value for DM Autoantibody Panel:
- Less than 1:4 titer with no antibody detected
Increased levels may indicate:
- Allergies to insulin
- Factitious hypoglycemia
- Insulin resistance
- Type I diabetes mellitus/ Insulin-dependent diabetes mellitus
Lipoprotein Profile (Lipid Profile) Normal Lab Values
Lipid assessment or lipid profile includes total cholesterol, high-density lipoprotein (HDL), low-density lipoprotein (LDL), and triglycerides.
- Cholesterol is present in all body tissues and is a major component of LDL, brain, and nerve cells, cell membranes, and some gallbladder stones.
- Triglycerides constitute a major part of very-low-density lipoproteins and a small part of LDLs. Increased cholesterol levels, LDL levels, and triglyceride levels place the client at risk for coronary artery disease. HDL helps protect against the risk of coronary artery disease.
Normal and critical lab values for Lipid Profile:
| Range (SI Units) | Range (Conventional) | |
|---|---|---|
| Cholesterol | ||
| Adult | <5.20 mmol/L | <200 mg/dL |
| Child | 3.1—5.2 mmol/L | 120—200 mg/dL |
| Infant | 1.8—4.5 mmol/L | 70—175 mg/dL |
| Newborn | 1.4—3.5 mmol/L | 53—135 mg/dL |
| High-density lipoprotein (HDL) | ||
| Male | >0.75 mmol/L | >45 mg/dL |
| Female | >0.91 mmol/L | >55 mg/dL |
| Low-density lipoprotein (LDL) | <3.4 mmol/L | <130 mg/dL |
| Very low-density lipoprotein (VLDL) | 0.18—0.83 mmol/L | 7—32 mg/dL |
| Triglycerides (TGs) | 0.45—1.81 mmol/L | 40—160 mg/dL |
| Critical values (TGs) | >4.5 mmol/L | >400 mg/dL |
High-density lipoprotein (HDL)
Increased HDL levels may indicate:
- Extensive exercise
- Familial HDL lipoproteinemia
Decreased HDL levels may indicate:
- Familial low HDL
- Hepatocellular disease (e.g., cirrhosis or hepatitis)
- Hypoproteinemia (e.g.,malnutrition or nephrotic syndrome)
- Metabolic syndrome
Low-density lipoprotein (LDL) and Very-low-density lipoprotein (VLDL)
Increased LDL and VLDL levels may indicate:
- Alcohol consumption
- Apoprotein CII deficiency
- Chronic liver disease
- Cushing's syndrome
- Familial hypercholesterolemia type IIa
- Familial LDL lipoproteinemia
- Gammopathies (e.g., multiple myeloma)
- Glycogen storage disease (e.g., von Gierke's disease)
- Hepatoma
- Hypothyroidism
- Nephrotic syndrome
Decreased LDL and VLDL Levels may indicate:
- Familial hypolipoproteinemia
- Hyperthyroidism
- Hypoproteinemia (e.g., severe burns, malnutrition, or malabsorption)
Nursing Considerations
- Oral contraceptives may increase the lipid level.
- Instruct the client to abstain from foods and fluid, except for water, for 12 to 14 hours and from alcohol for 24 hours before the test.
- Instruct the client to avoid consuming high-cholesterol foods with the evening meal before the test.
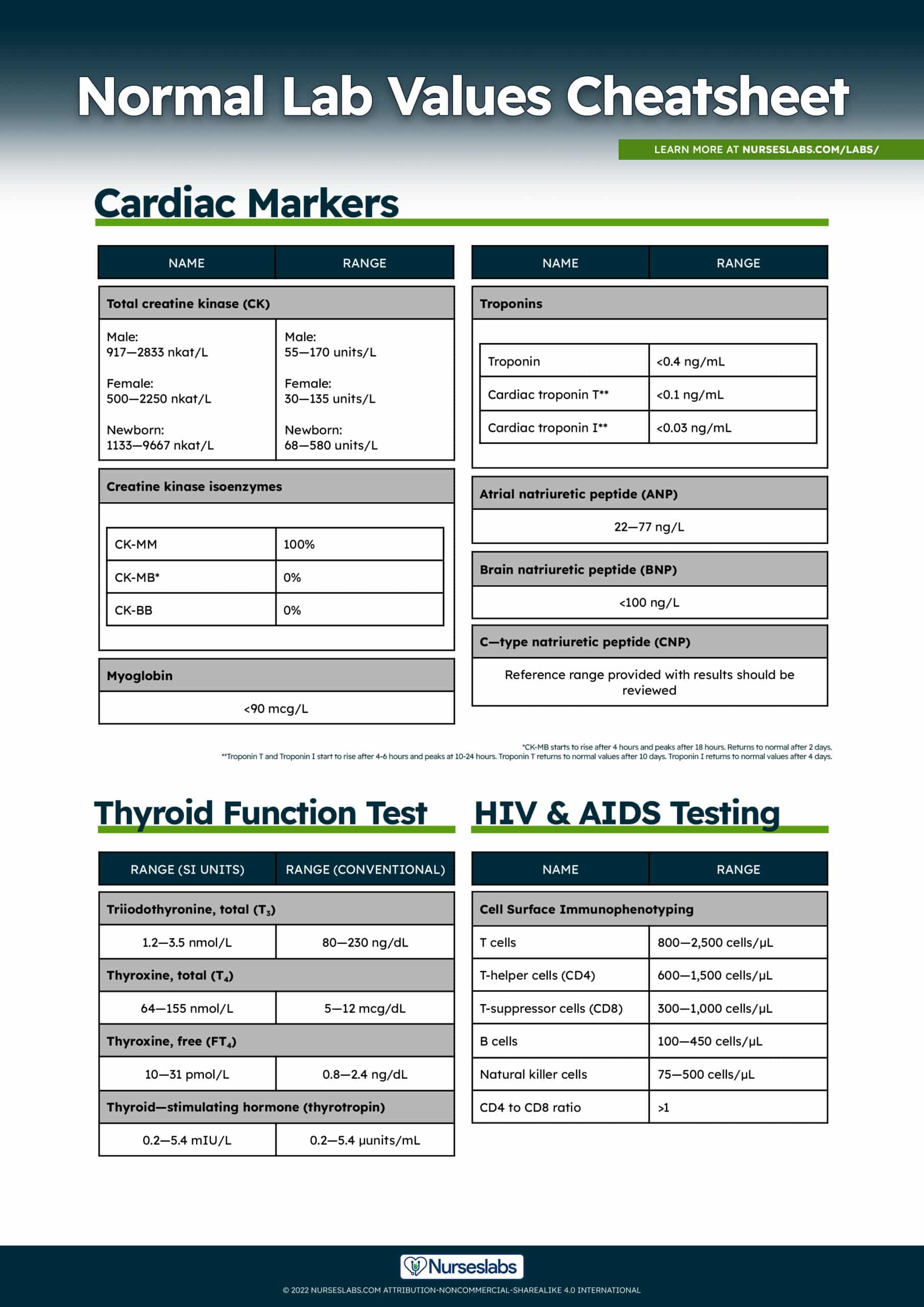
Cardiac Markers and Serum Enzymes
Serum enzymes and cardiac markers are released into the circulation normally following a myocardial injury as seen in acute myocardial infarction (MI) or other conditions such as heart failure.
Creatine Kinase (CK)
Creatine kinase (CK) is an enzyme found in muscle and brain tissue that reflects tissue catabolism resulting from cell trauma. The CK level begins to rise within 6 hours of muscle damage, peaks at 18 hours, and returns to normal in 2 to 3 days. The test for CK is performed to detect myocardial or skeletal muscle damage or central nervous system damage. Isoenzymes include CK-MB (cardiac), CK-BB (brain), and CK-MM (muscles):
- CK-MM is found mainly in skeletal muscle.
- CK-MB is found mainly in cardiac muscle
- CK-BB is found mainly in brain tissue
Normal values for total creatine kinase (CK):
| Range (SI Units) | Range (Conventional) | |
|---|---|---|
| Male | 917—2833 nkat/L | 55—170 units/L |
| Female | 500—2250 nkat/L | 30—135 units/L |
| Newborn | 1133—9667 nkat/L | 68—580 units/L |
Normal values for total CK isoenzymes:
| Normal Range | |
|---|---|
| CK-MM | 100% |
| CK-MB | 0% |
| CK-BB | 0% |
Increased levels of total creatine phosphokinase (CPK):
- Disease or injury affecting the brain, heart muscle, and skeletal muscle
Increased levels of CPK-BB isoenzyme:
- Adenocarcinoma (breast and lungs)
- Disease involving the central nervous system
- Pulmonary infarction
Increased levels of CPK-MB isoenzyme:
- Acute myocardial infarction
- Cardiac aneurysm surgery
- Cardiac defibrillation
- Cardiac ischemia
- Myocarditis
- Ventricular arrhythmias
Increased levels of CPK-MM isoenzyme:
- Crush injuries
- Delirium tremens
- Electroconvulsive therapy
- Electromyography
- Hypokalemia
- Hypothyroidism
- IM injections
- Malignant hyperthermia
- Muscular dystrophy
- Myositis
- Recent convulsions
- Recent surgery
- Rhabdomyolysis
- Shock
- Trauma
Nursing Considerations
- If the test is to evaluate skeletal muscle, instruct the client to avoid strenuous physical activity for 24 hours before the test.
- Instruct the client to avoid ingestion of alcohol for 24 hours before the test.
- Invasive procedures and intramuscular injections may falsely elevate CK levels.
Myoglobin
Myoglobin, an oxygen-binding protein that is found in striated (cardiac and skeletal) muscle, releases oxygen at very low tensions. Any injury to skeletal muscle will cause a release of myoglobin into the blood. Myoglobin rise in 2-4 hours after an MI making it an early marker for determining cardiac damage.
Normal Lab Values for Myoglobin
| Myoglobin |
|---|
| 5—70 ng/mL |
Myoglobin
Increased myoglobin levels:
- Malignant hyperthermia
- Muscular dystrophy
- Myocardial infarction
- Myositis
- Rhabdomyolysis
- Skeletal muscle ischemia
- Skeletal muscle trauma
Nursing Considerations
- The level can rise as early as 2 hours after a myocardial infarction, with a rapid decline in the level after 7 hours.
- Because the myoglobin level is not cardiac specific and rises and falls so rapidly, its use in diagnosing myocardial infarction may be limited.
Troponin I and Troponin T
Troponin is a regulatory protein found in striated muscle (myocardial and skeletal). Increased amounts of troponin are released into the bloodstream when an infarction causes damage to the myocardium. Troponin levels are elevated as early as 3 hours after MI. Troponin T and Troponin I start to rise after 4-6 hours and peaks at 10-24 hours. Troponin T returns to normal values after 10 days. Troponin I returns—normal values after 4 days. Serial measurements are important to compare with a baseline test; elevations are clinically significant in the diagnosis of cardiac pathology.
Normal values for Troponins:
| Normal Range | |
|---|---|
| Troponin | <0.4 ng/mL |
| Cardiac troponin T* | <0.1 ng/mL |
| Cardiac troponin I* | <0.03 ng/mL |
Increased troponin levels may indicate:
- Myocardial infarction
- Myocardial injury
Nursing Considerations
- Rotate venipuncture sites.
- Testing is repeated in 12 hours or as prescribed, followed by daily testing for 3 to 5 days.
Natriuretic Peptides
Natriuretic peptides are neuroendocrine peptides that are used to identify clients with heart failure. There are three major peptides:
- atrial natriuretic peptides (ANP) synthesized in cardiac ventricle muscle,
- brain natriuretic peptides (BNP) synthesized in the cardiac ventricle muscle
- C-type natriuretic peptides (CNP) synthesized by endothelial cells.
BNP is the primary marker for identifying heart failure as the cause of dyspnea. The higher the BNP level, the more severe the heart failure. If the BNP level is elevated, dyspnea is due to heart failure; if it is normal, the dyspnea is due to a pulmonary problem.
Normal values for Natriuretic Peptides:
| Normal Range | |
|---|---|
| Atrial natriuretic peptide (ANP) | 22—77 ng/L |
| Brain natriuretic peptide (BNP) | <100 ng/L |
| C-type natriuretic peptide (CNP) | Reference range provided with results should be reviewed |
Natriuretic peptides
Increased natriuretic peptides levels:
- Congestive heart failure
- Cor pulmonale
- Heart transplant rejection
- Myocardial infarction
- Systemic hypertension
Nursing Considerations
- Fasting is not required.
HIV and AIDS Testing
The following laboratory tests are used to diagnose human immunodeficiency virus (HIV), which is the cause of acquired immunodeficiency syndrome (AIDS). Common tests used to determine the presence of antibodies to HIV include ELISA, Western blot, and Immunofluorescence assay (IFA).
- A single reactive ELISA test by itself cannot be used to diagnose HIV and should be repeated in duplicate with the same blood sample; if the result is repeatedly reactive, follow-up tests using Western blot or IFA should be performed.
- A positive Western blot or IFA results is considered confirmatory for HIV.
- A positive ELISA result that fails to be confirmed by Western blot or IFA should not be considered negative, and repeat testing should take place in 3 to 6 months.
CD4+ T-cell counts
CD4+ T-cell counts help Monitors the progression of HIV. As the condition progresses, usually the number of CD4+ T-cells decreases, with a resultant decrease in immunity. In general, the immune system remains healthy with CD4+ T-cell counts higher than 500 cells/L. Immune system problems occur when the CD4+ T-cell count is between 200 and 499 cells/L. Severe immune system problems occur when the CD4+ T-cell count is lower than 200 cells/L.
Normal values for HIV and AIDS Testing:
| Normal Range | |
|---|---|
| T cells | 800—2,500 cells/µL |
| T-helper cells (CD4) | 600—1,500 cells/µL |
| T-suppressor cells (CD8) | 300—1,000 cells/µL |
| B cells | 100—450 cells/µL |
| Natural killer cells | 75—500 cells/µL |
| CD4—CD8 ratio | >1 |
Increased CD4+ T-cell counts may indicate:
- B-cell lymphoma
- T-cell lymphoma
- Chronic lymphatic leukemia
Decreased CD4+ T-cell counts may indicate:
- Congenital immunodeficiency
- HIV-positive patients
- Organ transplants
Thyroid Studies Normal Lab Values
Thyroid studies are performed if a thyroid disorder is suspected. Common laboratory blood tests such as thyroxine, TSH, T4, and T3 are done to evaluate thyroid function. Thyroid studies help differentiate primary thyroid disease from secondary causes and from abnormalities in thyroxine-binding globulin levels. Thyroid peroxidase antibodies test may be done to identify the presence of autoimmune conditions involving the thyroid gland.
Normal values for thyroid function tests:
| Range (SI Units) | Range (Conventional) | |
|---|---|---|
| Triiodothyronine, total (T3) | 1.2—3.5 nmol/L | 80—230 ng/dL |
| Thyroxine, total (T4) | 64—155 nmol/L | 5—12 µg/dL |
| Thyroxine, free (FT4) | 10—31 pmol/L | 0.8—2.4 ng/dL |
| Thyroid—stimulating hormone (thyrotropin) | 0.2—5.4 mIU/L | 0.2—5.4 µunits/mL |
Triiodothyronine (T₃)
Increased triiodothyronine levels may indicate:
- Acute thyroiditis
- Congenital hyperproteinemia
- Factitious hyperthyroidism
- Grave's disease
- Hepatitis
- Pregnancy
- Plummer's disease
- Struma ovarii
- Toxic thyroid adenoma
Decreased triiodothyronine levels may indicate:
- Cirrhosis
- Cretinism
- Cushing's syndrome
- Hypothalamic failure
- Hypothyroidism
- Iodine insufficiency
- Liver disease
- Myxedema
- Pituitary insufficiency
- Protein malnutrition and other protein-depleted states
- Renal failure
- Thyroid surgical ablation
Thyroxine (T₄)
Increased thyroxine levels may indicate:
- Acute thyroiditis
- Congenital hyperproteinemia
- Familial dysalbuminemic hyperthyroxinemia
- Factitious hyperthyroidism
- Grave's disease
- Hepatitis
- Pregnancy
- Plummer's disease
- Struma ovarii
- Toxic thyroid adenoma
Decreased thyroxine levels may indicate:
- Cirrhosis
- Cretinism
- Cushing's syndrome
- Hypothalamic failure
- Iodine insufficiency
- Myxedema
- Pituitary insufficiency
- Protein-depleted states
- Renal failure
- Surgical ablation
Thyroxine, free (FT₄)
Increased Thyroxine, free (FT₄) levels may indicate:
- Acute thyroiditis
- Congenital hyperproteinemia
- Familial dysalbuminemic hyperthyroxinemia
- Factitious hyperthyroidism
- Grave's disease
- Hepatitis
- Pregnancy
- Plummer's disease
- Struma ovarii
- Toxic thyroid adenoma
Decreased Thyroxine Levels may indicate:
- Cirrhosis
- Cretinism
- Cushing's syndrome
- Hypothalamic failure
- Iodine insufficiency
- Myxedema
- Pituitary insufficiency
- Protein-depleted states
- Renal failure
- Surgical ablation
Thyroid-stimulating hormone (thyrotropin)
Abnormal findings:
- Acute starvation
- Hyperthyroidism
- Hypothyroidism
- Old age
- Psychiatric primary depression
- Pregnancy
Nursing Considerations
- Results of the test may be invalid if the client has undergone a radionuclide scan within 7 days before the test.
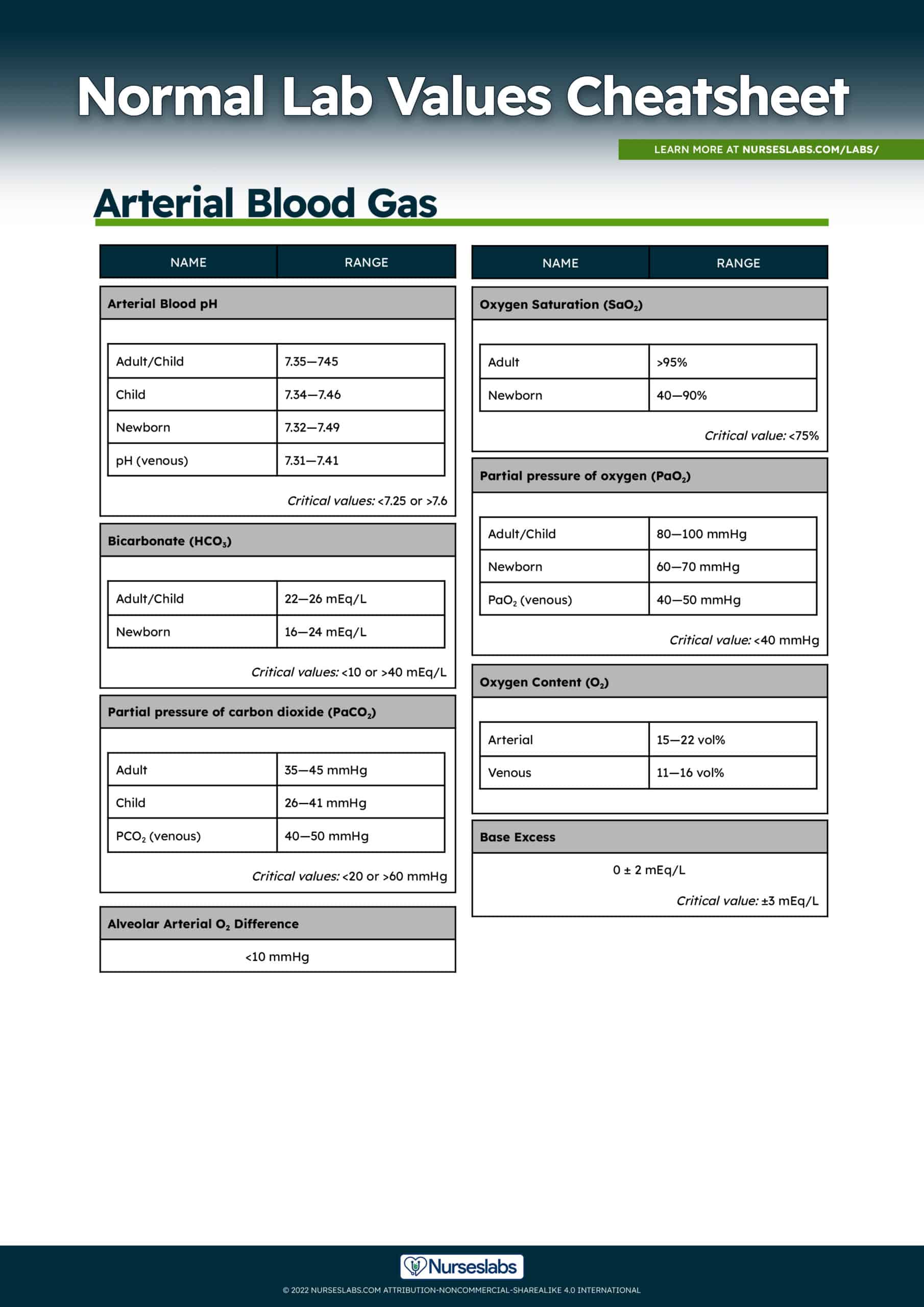
Arterial Blood Gas (ABG) Normal Lab Values
Arterial Blood Gases (ABGs) are measured in a laboratory test to determine the extent of compensation by the buffer system. It measures the acidity (pH) and the levels of oxygen and carbon dioxide in arterial blood. Blood for an ABG test is taken from an artery whereas most other blood tests are done on a sample of blood taken from a vein. To help you interpret ABG results, check out our 8-Step Guide to ABG Analysis Tic-Tac-Toe Method.
Normal values for arterial blood gasses (ABG):
| Range (SI Units) | |
|---|---|
| Arterial Blood pH | |
| Adult/Child | 7.35—745 |
| Newborn | 7.32—7.49 |
| ph (Venous) | 7.31—7.41 |
| Critical values (pH): | <7.25 or >7.6 |
| Partial pressure of carbon dioxide (PaCO2) | |
| Adult | 35—45 mmHg |
| Child | 26—41 mmHg |
| PCO2 (venous) | 40—50 mmHg |
| Critical values (PCO2 ) | <20 or >60 mmHg |
| Bicarbonate (HCO3) | |
| Adult/Child | 22—26 mEq/L |
| Newborn | 16—24 mEq/L |
| Critical values (HCO3) | <10 or >40 mEq/L |
| Partial pressure of oxygen (PaO2) | |
| Adult | 80—100 mmHg |
| Newborn | 60—70 mmHg |
| PaO2 (venous) | 40—50 mmHg |
| Critical value (PaO2) | <40 mmHg |
| Oxygen Saturation (SaO2) | |
| Adult | >95% |
| Newborn | 40—90% |
| Critical value (SaO2) | <75% |
| Oxygen Content (O2) | |
| Arterial | 15—22 vol% |
| Venous | 11—16 vol% |
| Base Excess | |
| Base Excess Normal | 0 ± 2 mEq/L |
| Critical value (Base Excess) | ±3 mEq/L |
| Alveolar Arterial O2 Difference | <10 mmHg |
Increased pH levels (Alkalosis)
Metabolic alkalosis may indicate:
- Aldosteronism
- Chronic vomiting
- Chronic and high-volume gastric suction
- Hypochloremia
- Hypokalemia
- Mercurial diuretics
Respiratory alkalosis may indicate:
- Acute and severe pulmonary disease
- Anxiety neuroses
- Carbon monoxide poisoning
- Chronic heart failure
- Cystic fibrosis
- Pain
- Pregnancy
- Pulmonary emboli
- Shock
Decreased pH (Acidosis)
Metabolic acidosis may indicate:
- Ketoacidosis
- Lactic acidosis
- Renal failure
- Severe diarrhea
Respiratory acidosis may indicate:
- Respiratory failure
Pco2
Increased Pco2 levels may indicate:
- Chronic obstructive pulmonary disease
- Head trauma
- Overoxygenation in a patient with COPD
- Oversedation
- Pickwickian syndrome
Decreased Pco2 levels may indicate:
- Anxiety
- Hypoxemia
- Pain
- Pregnancy
- Pulmonary emboli
Po2 and O2 content
Increased Po2,increased O2 content may indicate:
- Hyperventilation
- Increased inspired O2
Decreased Po2,increased O2 content may indicate:
- Adult respiratory distress syndrome
- Anemias
- Atelectasis
- Atrial or ventricular cardiac septal defects
- Bronchospasm
- Emboli
- Inadequate oxygen in inspired air (suffocation)Mucus plug
- Pneumothorax
- Pulmonary edema
- Restrictive lung disease
- Severe hypoventilation (e.g., neurologic somnolence, oversedation)
HCO3
Increased HCO3 levels may indicate:
- Aldosteronism
- Chronic and high-volume gastric suction
- Chronic vomiting
- Chronic obstructive pulmonary disease
- Use of mercurial diuretics
Decreased HCO3 levels may indicate:
- Acute renal failure
- Chronic and severe diarrhea
- Chronic use of loop diuretics
- Diabetic ketoacidosis
- Starvation
Hepatitis Testing
Serological tests for specific hepatitis virus markers assist in determining the specific type of hepatitis. Tests for hepatitis include radioimmunoassay, enzyme-linked immunosorbent assay (ELISA), and microparticle enzyme immunoassay.
Reference guide for hepatitis testing:
- Hepatitis A: Presence of immunoglobulin M (IgM) antibody to Hepatitis A and presence of total antibody (IgG and IgM) may suggest recent or current Hep A infection.
- Hepatitis B: Detection of Hep B core Antigen (HBcAg), envelope antigen (HBeAg), and surface antigen (HBsAg), or their corresponding antibodies.
- Hepatitis C: Confirmed by the presence of antibodies to Hep C virus.
- Hepatitis D: Detection of Hep D antigen (HDAg) early in the course of infection and detection of Hep D virus antibody in later stages of the disease.
- Hepatitis E: Specific serological tests for hepatitis E virus include detection of IgM and IgG antibodies to hepatitis E.
Nursing Considerations
- If the radioimmunoassay technique is being used, the injection of radionuclides within 1 week before the blood test is performed may cause falsely elevated results.
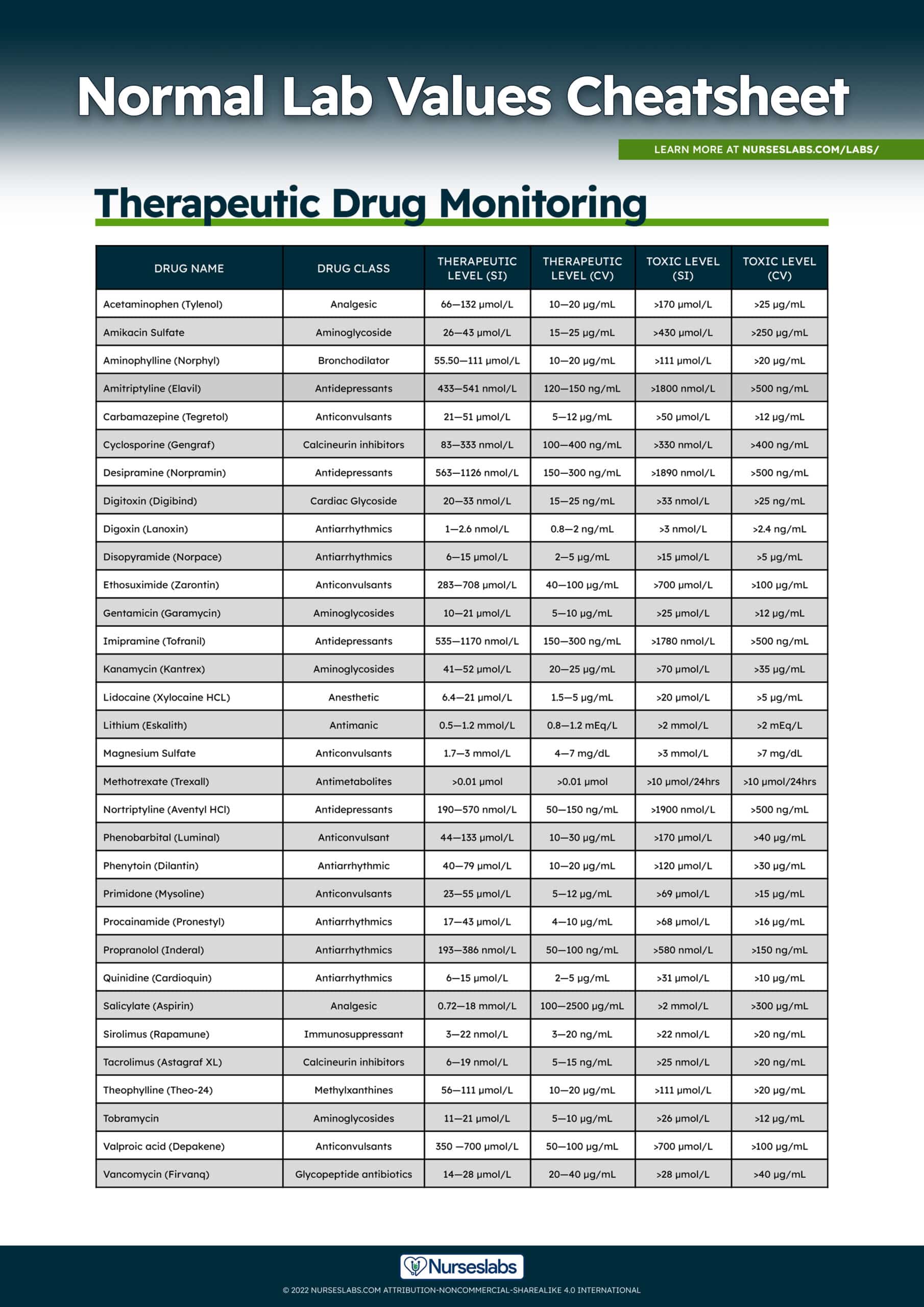
Therapeutic Drug Monitoring Normal Lab Values
Monitoring the therapeutic levels of certain medications is often conducted when the patient is taking medications with a narrow therapeutic range where a slight imbalance could be critical. Drug monitoring includes drawing blood samples for peak and trough levels to determine if blood serum levels of a specific drug are at a therapeutic level and not a subtherapeutic or toxic level. The peak level indicates the highest concentration of the drug in the blood serum while the trough level represents the lowest concentration. The following are the normal therapeutic serum medication levels:
| Drug Name | Drug Class | Therapeutic Level (SI) | Therapeutic Level (CV) | Toxic Level (SI) | Toxic Level (CV) |
|---|---|---|---|---|---|
| Acetaminophen (Tylenol) | Analgesic | 66—132 µmol/L | 10—20 µg/mL | >170 µmol/L | >25 µg/mL |
| Amikacin Sulfate | Aminoglycoside | 26—43 µmol/L | 15—25 µg/mL | >430 µmol/L | >250 µg/mL |
| Aminophylline (Norphyl) | Bronchodilator | 55.50—111 µmol/L | 10—20 µg/mL | >111 µmol/L | >20 µg/mL |
| Amitriptyline (Elavil) | Antidepressants | 433—541 nmol/L | 120—150 ng/mL | >1800 nmol/L | >500 ng/mL |
| Carbamazepine (Tegretol) | Anticonvulsants | 21—51 µmol/L | 5—12 µg/mL | >50 µmol/L | >12 µg/mL |
| Cyclosporine (Gengraf) | Calcineurin inhibitors | 83—333 nmol/L | 100—400 ng/mL | >330 nmol/L | >400 ng/mL |
| Desipramine (Norpramin) | Antidepressants | 563—1126 nmol/L | 150—300 ng/mL | >1890 nmol/L | >500 ng/mL |
| Digitoxin (Digibind) | Cardiac Glycoside | 20—33 nmol/L | 15—25 ng/mL | >33 nmol/L | >25 ng/mL |
| Digoxin (Lanoxin) | Antiarrhythmics | 1—2.6 nmol/L | 0.8—2 ng/mL | >3 nmol/L | >2.4 ng/mL |
| Disopyramide (Norpace) | Antiarrhythmics | 6—15 µmol/L | 2—5 µg/mL | >15 µmol/L | >5 µg/mL |
| Ethosuximide (Zarontin) | Anticonvulsants | 283—708 μmol/L | 40—100 µg/mL | >700 μmol/L | >100 µg/mL |
| Gentamicin (Garamycin) | Aminoglycosides | 10—21 µmol/L | 5—10 µg/mL | >25 µmol/L | >12 µg/mL |
| Imipramine (Tofranil) | Antidepressants | 535—1170 nmol/L | 150—300 ng/mL | >1780 nmol/L | >500 ng/mL |
| Kanamycin (Kantrex) | Aminoglycosides | 41—52 µmol/L | 20—25 µg/mL | >70 µmol/L | >35 µg/mL |
| Lidocaine (Xylocaine HCL) | Anesthetic | 6.4—21 µmol/L | 1.5—5 µg/mL | >20 µmol/L | >5 µg/mL |
| Lithium (Eskalith) | Antimanic | 0.5—1.2 mmol/L | 0.8—1.2 mEq/L | >2 mmol/L | >2 mEq/L |
| Magnesium Sulfate | Anticonvulsants | 1.7—3 mmol/L | 4—7 mg/dL | >3 mmol/L | >7 mg/dL |
| Methotrexate (Trexall) | Antimetabolites | >0.01 µmol | >0.01 µmol | >10 µmol/24 hours | >10 µmol/24 hours |
| Nortriptyline (Aventyl HCl) | Antidepressants | 190—570 nmol/L | 50—150 ng/mL | >1900 nmol/L | >500 ng/mL |
| Phenobarbital (Luminal) | Anticonvulsant | 44—133 µmol/L | 10—30 µg/mL | >170 µmol/L | >40 µg/mL |
| Phenytoin (Dilantin) | Antiarrhythmic | 40—79 µmol/L | 10—20 µg/mL | >120 µmol/L | >30 µg/mL |
| Primidone (Mysoline) | Anticonvulsants | 23—55 µmol/L | 5—12 µg/mL | >69 µmol/L | >15 µg/mL |
| Procainamide (Pronestyl) | Antiarrhythmics | 17—43 µmol/L | 4—10 µg/mL | >68 µmol/L | >16 µg/mL |
| Propranolol (Inderal) | Antiarrhythmics | 193—386 nmol/L | 50—100 ng/mL | >580 nmol/L | >150 ng/mL |
| Quinidine (Cardioquin) | Antiarrhythmics | 6—15 µmol/L | 2—5 µg/mL | >31 µmol/L | >10 µg/mL |
| Salicylate (Aspirin) | Analgesic | 0.72—18 mmol/L | 100—2500 µg/mL | >2 mmol/L | >300 µg/mL |
| Sirolimus (Rapamune) | Immunosuppressant | 3—22 nmol/L | 3—20 ng/mL | >22 nmol/L | >20 ng/mL |
| Tacrolimus (Astagraf XL) | Calcineurin inhibitors | 6—19 nmol/L | 5—15 ng/mL | >25 nmol/L | >20 ng/mL |
| Theophylline (Theo-24) | Methylxanthines | 56—111 µmol/L | 10—20 µg/mL | >111 µmol/L | >20 µg/mL |
| Tobramycin | Aminoglycosides | 11—21 µmol/L | 5—10 µg/mL | >26 µmol/L | >12 µg/mL |
| Valproic acid (Depakene) | Anticonvulsants | 350 —700 µmol/L | 50—100 µg/mL | >700 µmol/L | >100 µg/mL |
| Vancomycin (Firvanq) | Glycopeptide antibiotics | 14—28 µmol/L | 20—40 µg/mL | >28 µmol/L | >40 µg/mL |
How to Obtain a Blood Sample
A phlebotomist or a nurse with training and certification in collecting a blood sample are allowed to perform venipuncture for the purpose of blood specimen collection. These are the steps to follow in obtaining a blood sample:
- Identify the client. Accurately identify the client by asking his or her name and birthdate; Explain the reason for the test and procedure to the client.
- Proper position. Blood samples should be drawn in a sitting position and the client should remain in that position for at least 5 minutes before the blood collection.
- Confirm the request. Check the laboratory form for the ordered test, client information, and additional requirements (fasting, dietary restrictions, medications).
- Provide comfort. Make sure the client remove any tight clothing that might constrict the upper arm. The arm is placed in a downward position supported on the armrest.
- Ensure proper hand hygiene. Perform hand washing before putting on non-latex gloves.
- Identify the vein. Examine the client's arm to select the most easily accessible vein for venipuncture then place the tourniquet 3 to 4 inches above the chosen site. Do not place the tourniquet tightly or leave on more than 2 minutes.
- Prepare the site. When a vein is chosen, cleanse the area using alcohol in a circular motion beginning at the site and working toward.
- Draw the sample. Ask the client to make a fist. Grasp the client's arm firmly using your thumb to draw the skin taut and anchor the vein from rolling. Gently insert the needle at a 15 to 30º angle through the skin and into the lumen of the vein.
- Fill the tube. Obtain the needed amount of blood sample, then release and remove the tourniquet.
- Remove the needle. In a swift backward motion, remove the needle from the client's arm. and apply a folded gauze over the venipuncture site for 1 to 2 minutes.
- Label the tube. Label the tube with the client's name, date of birth, hospital number, date and time of the collection.
- Transport specimen. Deliver the specimen to the laboratory for immediate processing and analysis.
References and Sources
Suggested reading and additional resources for this Normal Laboratory Values guide:
- Corbett, J. V., & Banks, A. (2018).Laboratory Tests and Diagnostic Procedures with Nursing Diagnoses with Nursing Diagnoses. Pearson Education. [Link]
- Kratz, A., & Lewandrowski, K. B. (1998). Normal reference laboratory values.New England Journal of Medicine,339(15), 1063-1072. [Link]
- Kratz, A., Ferraro, M., Sluss, P. M., & Lewandrowski, K. B. (2004). Laboratory reference values.New England Journal of Medicine,351, 1548-1564. [Link]
Source: https://nurseslabs.com/normal-lab-values-nclex-nursing/
0 Response to "Easy Way to Learn Nursing Lab Values"
Post a Comment